Onubha Hoque Syed, Department of Global Sustainable Development, University of Warwick
Greater social research aiming to understand the qualitative experiences of patients and healthcare workers is necessary in order to create informed health policies. A key aspect of this is acknowledging and uncovering how 'lay' and 'expert' medical knowledge interact and co-exist. This paper uses the context of fever treatment in Yangon, Myanmar, to investigate the factors behind differences between 'lay' and 'expert' medical knowledge.
This cross-sectional study conducts a deductive thematic analysis of secondary qualitative data from both patients and medical doctors using an adapted form of Amartya Sen's capability approach framework. Results uncover how education, socially rooted collective knowledge and unregulated pharmacies drive differences between 'lay' and 'expert' medical knowledge.
The results of this paper highlight the interdisciplinary nature of health, meaning health systems should be considered within their sociological, political and economic contexts. Appreciating the complexity of how health is understood by populations can allow policymakers to form a stronger health system by creating contextualised policies and health interventions for the general public that cater to the diversity of narratives within health systems and beliefs.
Keywords: Social medicine, expert biomedical knowledge in fever treatment, layman beliefs in medicine, traditional Burmese medicine, capability approach, Myanmar.
There has been great interest in social literature to better understand 'layman' beliefs of treatment and medicine. This interest may stem from the changes occurring in the interactions between 'expert' and 'lay' actors within health systems. The importance of patient narratives in diagnosing illnesses had been reduced during the rise of biomedicine in the nineteenth century. The increased use of laboratories and modern hospitals aided the conceptual separation of patients from their illnesses, meaning 'expert' translation was increasingly essential for patients to understand their bodies (Bury, 2001: 266). During the late twentieth century, however, greater emphasis was placed on healthcare workers to be more open to 'lay' beliefs than previously. Consequently, social research has been interested in uncovering what 'lay' knowledge can offer to different understandings of health (Prior, 2003: 43). However, 'lay' beliefs should not be considered in isolation, as patient knowledge and treatment preferences are heavily influenced by 'expert' healthcare workers and healthcare institutions (McClean and Shaw, 2005: 746; Lambert et al., 2019). Therefore, this paper examines 'lay' medical knowledge in conjunction with 'expert' medical knowledge to investigate what drives the differences in the two discourses. This expansive area of research is significant because when the qualitative experiences of healthcare workers and patients are not recognised as credible sources of knowledge, their social power to influence public policy is diminished. Thus, these actors may be deprived of their entitled share of collective financial and medical resources (Moes et al., 2020: 2).
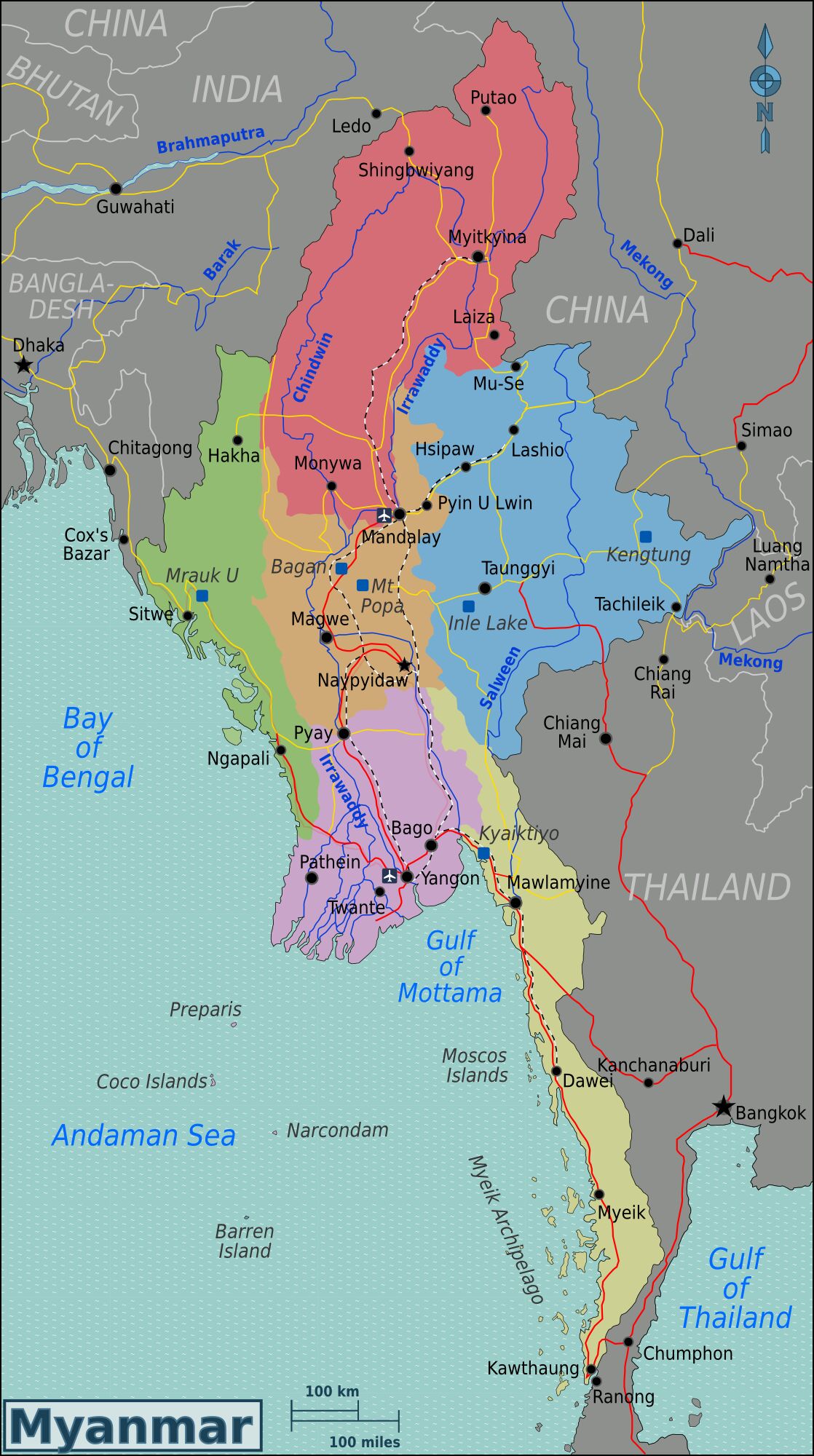
Myanmar (Figure 1) was chosen as the geographical focus of this paper as traditional medical practices are thriving in both public and private sectors (Sein et al., 2014: 32). Additionally, Yangon (the second-largest city in Myanmar) is where biomedicine is most widely available relative to all regions/states in the country. This is exemplified by Yangon having the highest number of total hospital beds (10,249) available in primary, secondary and tertiary curative care out of all the Burmese regions/states in 2012, as well as having the highest rate of delivery in healthcare facilities at 69 per cent (Sein et al., 2014). Thus, Yangon provides a context of both biomedical and traditional medical discourses, both relatively plentiful in supply, existing together.
When discussing 'expert' knowledge, this research is referring to biomedical knowledge – which, in the context of Yangon, is also referred to as 'Western'. Biomedical knowledge / biomedicine denotes the branch of medicine based principally on biology (Oxford English Dictionary, 2020). It has become the dominant medical discourse around the world, in part due to most governments using biomedicine to decide on health matters (Wiseman, 2004). In contrast, 'lay' knowledge in this paper is referring to the views, knowledge, beliefs and understanding of patients (Prior, 2003) and context-specific collective knowledge. This includes the use of Burmese traditional medicine, defined as national medicine shaped by Myanmar's culture, customs, traditions and geography (Shwe, 2010, cited in Coderey, 2021: 524). Although traditional medicine is a medical discourse in its own right, its use is included under the theme of socially derived lay knowledge in this research since traditional medicine can be seen as intertwined with social and familial networks. As a result, while there seems to be a distinction between traditional medicine and lay knowledge, the relationship between the two warrants the inclusion of references to traditional medicine to be included under themes relating to lay knowledge in this study.
This paper seeks to investigate the dynamics between 'lay' and 'expert' medical knowledge within a context of multiple medical discourses that co-exist in order to highlight how potentially contrasting understandings of health and treatment coincide. The secondary dataset analysed in this paper is on the treatment of fever at a primary-care level. The original study occurred alongside a clinical trial for diagnostic biomarker testing, designed to reduce the prescribing of antibiotics. This context is noteworthy as participants were often asked about, or made reference to, their antibiotic use (as either patients using antibiotics or as doctors prescribing antibiotics), meaning the understanding and beliefs related to biomedical treatments for a fever from both 'lay' and 'expert' viewpoints were strongly discussed.
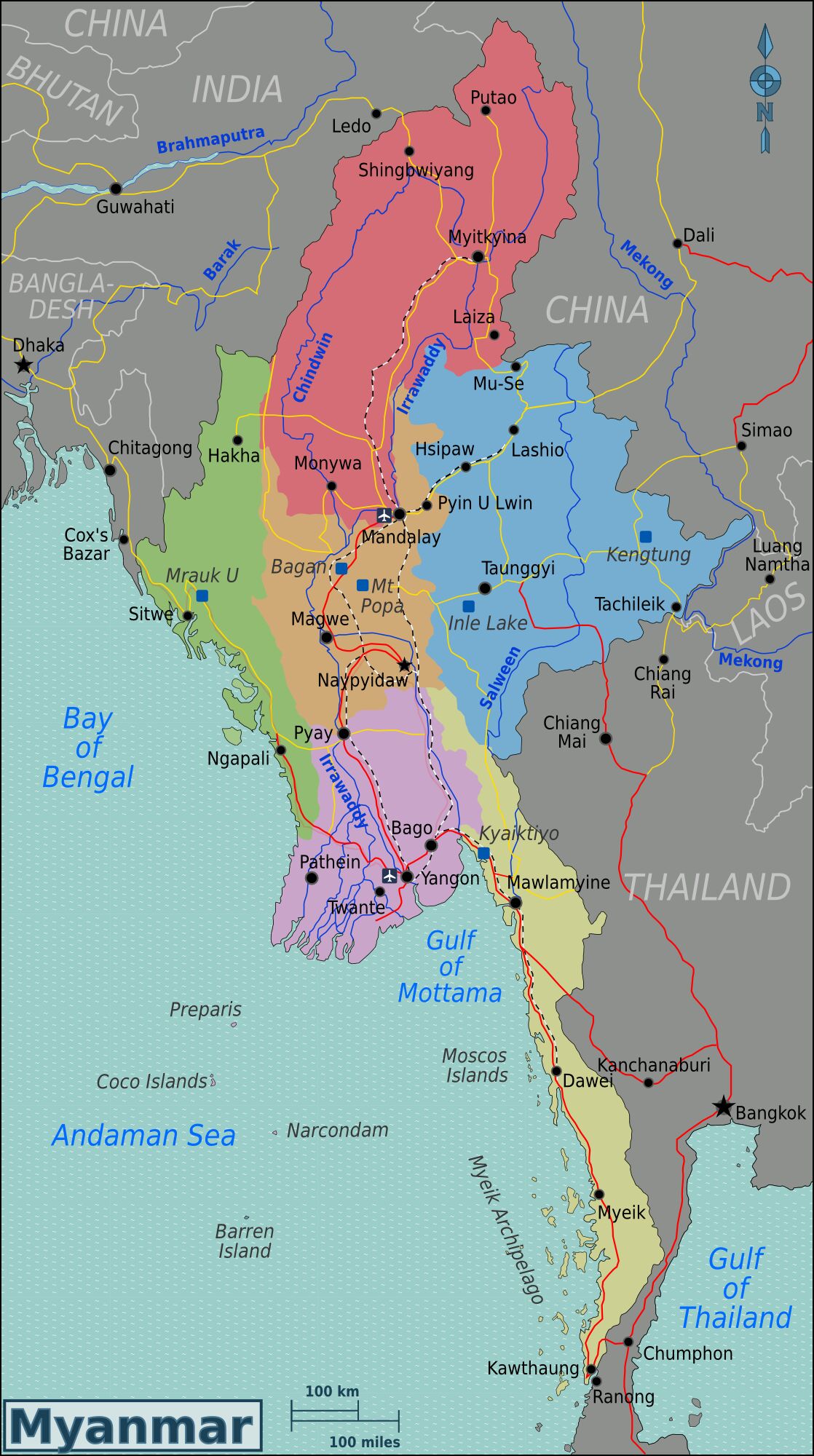
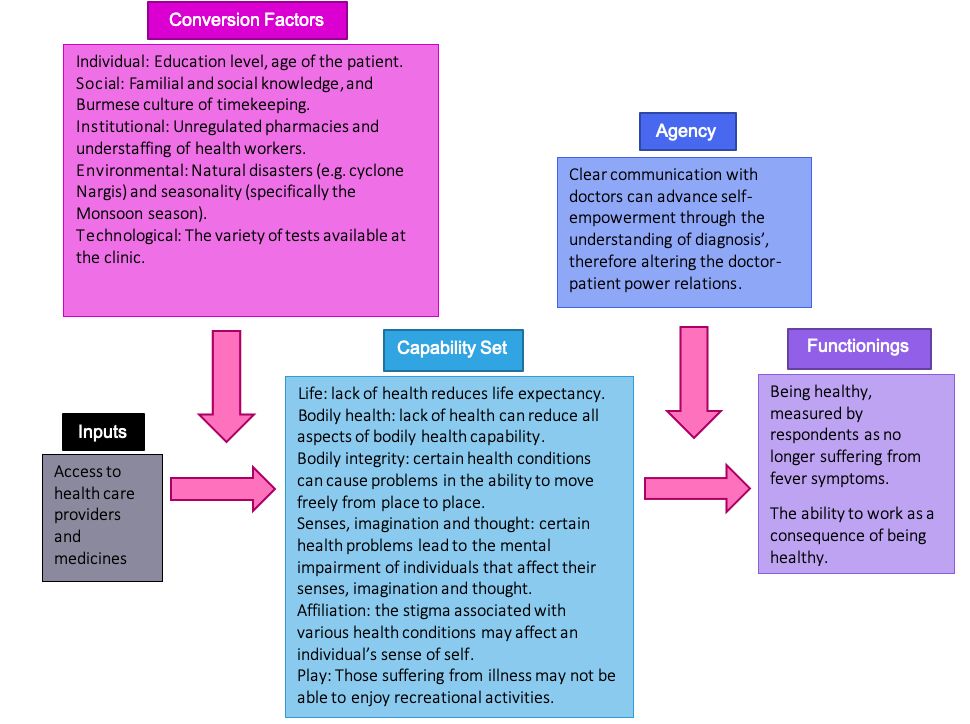
In order to investigate what factors are behind the differences between 'lay' and 'expert' medical knowledge, a capability approach framework (CAF) was applied; this was originally developed by economist Amartya Sen to measure standards of living (Figure 2). This framework measures a good standard of living as one where an individual has the opportunity to live life in the way they wish to.
The CAF is used to make assessments on the multi-dimensional wellbeing of individuals and to evaluate the impact of development practices on people (Haenssgen and Ariana, 2017; Robeyns 2005; Robeyns, 2006). It was chosen as the analytical framework for this research because, in its adapted form, it relays the experiences of key actors (healthcare workers and service users in this context) within health systems in their own words, while also capturing respondents' own definitions of health and wellbeing. Furthermore, the framework allows for greater appreciation of the interdisciplinary nature of health, including the multiple factors involved in accessing health services that exist outside of the health system.
Little literature exists on Burmese knowledge gaps in health, barring Thu et al. (2012) and Lwin et al. (2014) who used cross-sectional studies to assess knowledge of tuberculosis (TB) and malaria, respectively. Thu et al.'s study using a questionnaire, interviews and focus group discussions with factory workers in Yangon, Myanmar, to assess understandings of TB highlighted high levels of misconception surrounding TB transmission. Lwin et al. used a quantitative household survey to analyse the effectiveness of the Sun Primary Health (SPH) franchise programme on the diffusion of malaria knowledge by comparing the knowledge and health practices of those within and not within SPH intervention areas. Findings suggested that areas with SPH providers (volunteer health workers trained to give basic health services) had higher rates of malaria knowledge and were more likely to go to (biomedically) trained providers. While these are both valuable contributions to the literature, there is a distinctive lack of research using the CAF to understand 'lay' knowledge of health and treatment.
Peltzer et al. (2016) investigated the use of traditional medicine used by chronic disease patients in Myanmar; contrastingly, Khaing et al. (2015); Risso-Gill et al. (2013); Sommanustweechai et al. (2016) and Zaw et al. (2015) analysed Myanmar's health system and the disparities within it while maintaining a focus on biomedicine. The aforementioned literature, however, in its focus on a specific medical discourse fail to acknowledge the role of other medical discourses, despite Myanmar being heavily influenced by both biomedicine and traditional medicine.
Ariana and Naveed (2014) uniquely provide an excellent overview of how the capability approach can be used to investigate health outcomes by assessing how each component of the original capability approach can be translated to a factor impacting either the supply or demand for healthcare. This publication created the background for the adapted capability approach used in this paper. While Ariana and Naveed provide a meaningful contribution to the literature, there are still few examples of where the CAF has been applied to real-world health problems/context.
As a result of the limitations highlighted above, this research paper seeks to contribute to the literature the exposure of factors driving differences in 'lay' and 'expert' medical knowledge on fever treatment in Yangon, Myanmar. This was achieved by conducting a deductive thematic analysis of qualitative data, guided by the CAF. The CAF illustrated (Figure 2) was adapted to the context of fever treatment in Yangon to examine each stage of the treatment-seeking process from access to healthcare to being cured of a fever / relieved of symptoms.
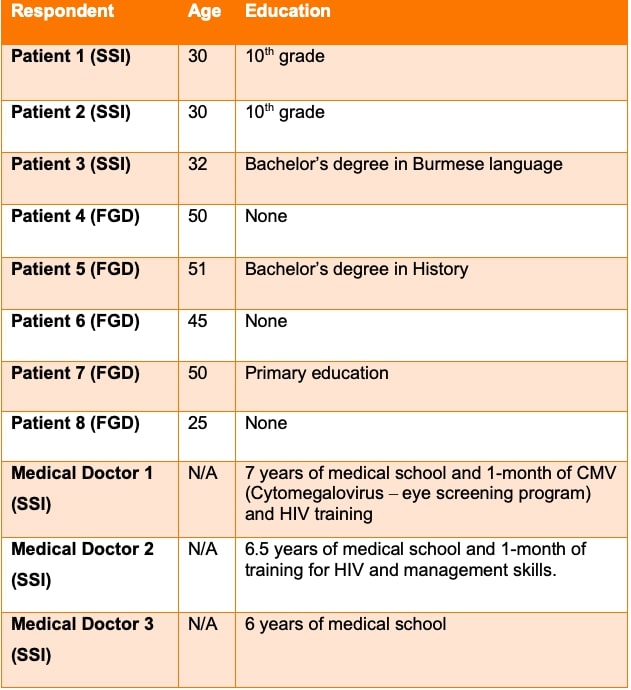
This research paper investigates the factors contributing to tensions between 'lay' and 'expert' medical knowledge in Yangon, Myanmar, through a cross-sectional study using secondary qualitative data on the treatment of fever in a hospital and clinics (including a free-of-charge non-governmental organisation (NGO) clinic) providing primary health services. Semi-structured interviews (SSIs) with medical doctors and female patients (or female guardians of patients) of the NGO clinic and from a focus group discussion (FGD) with female patients who visited other clinics and hospitals had been conducted between December 2016 and January 2017 (see Table 1).
The data analysed in this paper is part of the mixed-method research project 'The impact of C-reactive protein testing on antibiotic prescription in febrile patients attending primary care in low-resource settings', [1] whereby I build specifically on qualitative data collected under the leadership of Dr Marco J Haenssgen alongside a clinical trial of diagnostic biomarker tests to reduce antibiotic prescription on the primary-care level. For the qualitative data, written informed consent was obtained from all participants, and the research was approved by the University of Oxford Tropical Research Ethics Committee[2] and the Myanmar Department of Medical Research.[3] The analysis in this manuscript constitutes originally intended secondary qualitative work that has taken place under the supervision of the lead social scientist Dr Haenssgen, and therefore falls within the remit and intentions of the original social research to inform our understanding of patient–physician interactions in the context of antibiotic use in Yangon. The data analysed was thus fully anonymised to safeguard the participants and comprised a sub-sample of only female research participants to suit the scope of undergraduate coursework research. The full dataset is analysed in Haenssgen et al. (2019).
Originally, qualitative data from 130 interview and focus group participants across Myanmar, Thailand and Vietnam was collected alongside a clinical trial for C-reactive protein (CRP) biomarker testing. Respondents from Yangon in the original study were recruited from three clinics and one public hospital. The primary research team included native Burmese speakers, meaning translation errors were minimised. Detailed information on data collection and sampling in the primary study can be found in Haenssgen et al. (2019) and Zaw et al. (2018). CRP-biomarker testing intends to reduce the over-prescription of antibiotics at a primary-care level by using a finger-prick blood test to indicate whether a patient is likely to have a bacterial infection. Prescribing antibiotics are discouraged if a patient's test results are below a certain threshold, therefore indicating that the patient does not have a bacterial infection. Haenssgen et al.'s (2019) cross-case comparison study found that perceived infectious-disease risks, health-system factors and the demand-side context influenced the outcomes of the CRP-biomarker clinical trial. These results highlight the importance of appreciating context when designing anti-microbial resistance interventions.
The analysis of this paper differs from the original study – firstly, by it being a cross-sectional study rather than using the original cross-case comparison research design. This choice was made in order to focus on one context in particular detail. Secondly, this paper uses the CAF to guide thematic analysis, thereby using respondent-led understandings of health.
Deductive thematic analysis was conducted by utilising the CAF to extract and sort themes concerning the tensions between 'lay' and 'expert' medical knowledge. This process was repeated until data saturation was reached, defined as when no new or relevant information emerged. Reaching data saturation was made easier by the data sample being cohesive (relating specifically to patients and doctors undergoing or prescribing fever treatment within formal primary-care facilities in Yangon), as the findings from this study are not aiming to be transferrable to the general population (Fusch and Ness, 2015: 1413; Given, 2012). This method informs the research question as it analyses discourses surrounding the treatment of a fever from both patients and medical doctors, explained in their own words. Due to the resource constraints associated with undergraduate research, the researcher was solely involved in the coding of data.
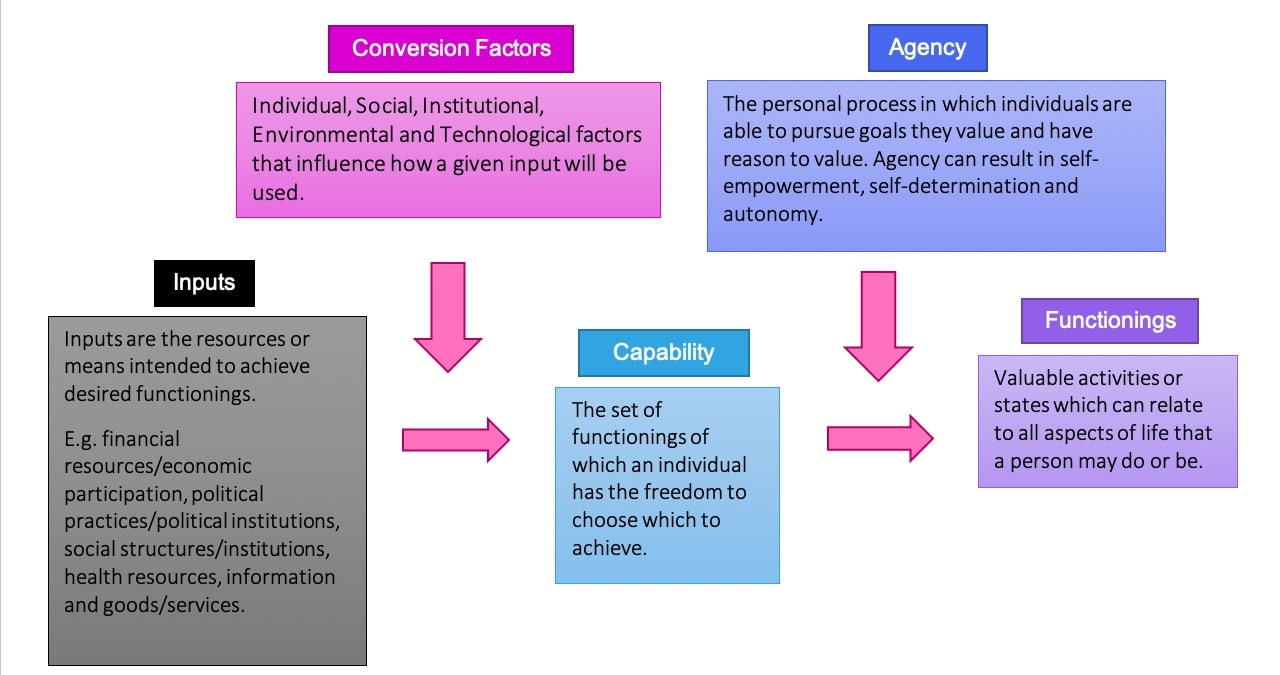
The results of thematic analysis are summarised in Figure 3 and expanded upon in this section.
Inputs
Access to healthcare providers and medicines is an input to the capability approach adapted to the realm of health (Ariana and Naveed, 2009) and can be seen in the context of Yangon, with most respondents living within close distance to a clinic:
From the house, it's about 10 minutes [by motorcycle]
Conversion factors:
Conversion factors that may change the way health inputs are used by individuals can be split into the following categories: individual, social, institutional, environmental and technological.
Individual
The age of the patient in question can determine how a fever is treated by patients. The following quote illustrates how guardians of children are more careful with treatment for children in comparison to themselves:
For myself, I take the medicine […] but for the kids […] we go to someone who knows better than us.
This may be due to a fear of the consequences that may arise by self-treating an illness using 'lay' knowledge.
The level of education of the patient was found to drive differences between 'expert' and 'lay' knowledge.
Social
A doctor described how the Burmese culture concerning timekeeping, which includes patients wanting to be first in receiving treatment, affects the service provided in clinics:
Burmese people, they want to be first in getting treatment, so they come in crowds as soon as the clinic opens […] that makes us stressed.
Being pressured by crowds of patients consequently makes consultation times shorter, meaning patients feel rushed and unable to ask questions concerning their diagnosis:
when [doctors] do check-ups […] [I] didn't even [have] time to ask [questions]
Therefore, this Burmese habit can reduce patient/'layman' understanding of the doctor's diagnosis / 'expert' biomedical knowledge.
Institutional
One institutional conversion factor is unregulated private pharmacies. This is where mixed medicines, antibiotics, Western medicines and traditional medicines can be bought at an out-of-pocket cost by consumers (Sein et al., 2014).
The critical understaffing of healthcare workers (Sommanustweechai et al., 2016), possibly due to the low salaries for public healthcare workers relative to costs of living (Sein et al., 2014) means doctors have excessive workloads, with only:
…four doctors for about 200 [patients].
This can contribute to the short interaction times between doctors and patients referred to in the social conversion factor section, in which patients feel unable to ask questions regarding their diagnosis:
[my doctor] couldn't stand on her feet and she fainted a lot [due to the high number of patients] […] she couldn't wait any longer [before moving on to the next patient], so we went [home].
As a result, differences between 'lay' and 'expert' medical knowledge can be driven by patients being unable to rely on 'expert' explanations of their illnesses or symptoms, as well as doctors being closed off from understanding 'lay' beliefs during this diagnosis period because of the limited interaction time between doctors and patients.
Environmental
Environmental factors bring differing levels of disease. Therefore, workload pressures vary seasonally:
during winter […] there is more upper respiratory infection […] and more flu. Summer [has] much less consultation overall.
In Monsoon it's more crowded […]. I have to examine faster […], so […] I am scared that I might miss out on something.
Natural disasters have similar impacts, such as when:
many moved […] to [redacted district name] after the cyclone Nargis and some would bring back their parents from their regions
Natural disasters consequently contribute to doctors' already burdening workload. Cyclone Nargis, the largest natural disaster in Myanmar's recent history, initially occurring 280km south-west of Yangon before working itself further inland, caused:
the destruction of 130 healthcare facilities […] and [had] a severe impact on the health system and its capacity to deliver essential services
Therefore, seasonality and natural disasters cause greater work pressure for doctors, longer waiting times discussed as both social and institutional conversion factors, and can significantly impact the ability of the healthcare system to deliver services. These impacts can all influence the diffusion of knowledge from 'expert' to 'layman' and vice versa as a consequence of reduced interaction between doctors and patients.
Technological
Patients felt that more testing constituted better treatment as there is more certainty in diagnosis:
When I [get tested], I know that they would give me something that is for my illness.
We get to know [if] there is a disease or not. I appreciate it.
Test results, therefore, enable a stronger belief in 'expert' diagnosis because patients feel that they have been thoroughly examined and accurately diagnosed. Doctors felt similarly; in the context of the CRP clinical trial, they shared that:
[if my] clinical assessment and the CRP test both matches and shows the need for antibiotic[s] […] then I have more confidence
Technology can provide confidence and certainty in 'expert' knowledge to both doctors and patients. With technology being unevenly spread through the health system, however, it can change the type of treatment provided to patients following their choice or option of clinic.
These individual, social, institutional, environmental and technological conversion factors highlight that the way 'lay' and 'expert' knowledge interact is highly dependent on the individual patient and doctor/clinic in question. Therefore, the social and environmental context heavily influences what differences may exist between the two discourses.
Capability set
The capability set used for this framework was adapted from the philosopher Martha Nussbaum's list of ten essential human capabilities. Nussbaum, one of the most influential scholars within the capability approach discourse, argues that these ten capabilities are essential for humans to enjoy a good standard of living (Alkire and Deneulin, 2009). Ariana and Naveed (2009) modified Nussbaum's list to the sphere of health (an edited version of six capabilities that are appropriate for the context provided by SSIs and the FDG is shown in Figure 3). This capability set encompasses several fundamental health goals that would contribute to a healthy and attainable standard of living in the context of Yangon.
Agency
Agency – concerning the individual process of achieving freedom that may involve/result in self-expression and autonomy – can be exercised through communication with healthcare workers. An example being when the guardian of a then seven-month-old patient felt treatment for a fever was not being correctly carried out:
I went to the Head of the Hospital and told him […] don't you have to change the cannula every week? Now the kid's leg […] [is] swollen and there is liquid coming out […]. Then the nurses got scolded […]. As soon as it came off, the kid [looked] more active.
The exercising of agency illustrates how 'lay' knowledge of the patient is communicated to the 'experts' during fever treatment, with the consequence being a movement beyond the typical paternalist doctor–patient relationship (Goodyear-Smith and Buetow, 2001).
Functionings
Having the characteristic of being only a functioning if the individual in question values the activity or state themselves, functionings identified from SSIs and the FGD were 'being healthy' and 'being able to work as a consequence of having a healthy body'. These functionings are exemplified by respondents:
A good treatment is when the symptoms we are feeling [are] somehow, relieved […].
It's because of health that we can work so the main importance is health.
These functionings indicate that as long as the symptoms of illness subside, the type of medical knowledge utilised for treatment (e.g. 'lay' knowledge as opposed to 'expert') is not of great importance.
In response to the research question of what factors are behind the differences between 'lay' and 'expert' medical knowledge in the context of fever treatment in Yangon, Myanmar, this study finds that the three main factors are: the education level of patients, familial knowledge passed down through generations and unregulated pharmacies.
Education
The education level of patients was persistently brought up by doctors as being a barrier to communicating 'expert' knowledge during diagnosis:
we have many patients who are non-educated, so when they give the history, it's not precise […] so then there is difficulty in giving medicines.
Additionally, post-consultation during the purchasing of medicine, a lack of formal education continues to prevent the diffusion of 'expert' knowledge to patients:
The medicine counter [gives the medicine] with instructions, but since they don't have much education, they might not understand it all. […]. Then some patients could [wrongly] take the medicine.
Following this lack of understanding of 'expert' knowledge:
Patients […] don't take [the] full course [of antibiotics]. No matter how much we explain it to them […]. It would be better if we could give [the public] a good education.
Although patients feel their diagnosis can be rushed at times (see social and institutional conversion factors), the above quotes suggest that time is not the only factor preventing adequate 'expert' explanation of patients' condition. A lack of formal education makes explaining a diagnosis to patients difficult for healthcare workers and makes it harder for patients to interpret 'expert' advice. The resulting miscommunication may be falsely identified as patients knowingly carrying out actions against doctor's advice and acting irrationally (especially at a policymaker level).
Social and familial knowledge
'Lay' knowledge can be linked to social or collective knowledge, with the use of traditional medicine being influenced by familial and social networks. This is exemplified by the following respondent:
[their great aunt] buys the Burmese medicine. There is the instruction written on it. [E.g.] stomach pains, gastric problems […] and if it correspond[s] to what I am feeling […] then I take it
The diffusion of traditional medicine, which is intertwined with socially produced 'lay' knowledge, is highlighted here:
[their great aunt recommends traditional medicine] to others and then they get better.
This illustrates the dispersion of traditional medicine as 'lay' knowledge because the respondent's great aunt shares treatment with their community, adding to or maintaining the pool of 'lay' knowledge.
Another respondent (a guardian of a patient) similarly shared their experience of the older generation of their family encouraging the use of traditional medicine in fever treatment, even if that respondent preferred biomedicine and would not necessarily use traditional methods themselves:
[the patient's] grandmother gave him a bath made from boiled betel leaves […] they said it [works]. Well, they are the elderly. As long as they don't feed him, I let them do it to make them happy.
This highlights the role of familial obligations and dynamics in 'layman' treatment using traditional medicine, and how the diffusion of 'lay' knowledge may be socially rooted.
Unregulated pharmacies
Unregulated pharmacies are another source of 'expert' knowledge in the sphere of health. However, due to the lax enforcement of regulations and a lack of adherence to the qualifications needed to run pharmacies (Sein et al., 2014), the information provided by unregulated pharmacies can be misleading or incorrect. The confusion this can cause patients by impacting their 'lay' understanding of illness is exemplified by the following experience of a respondent:
the clinic gave me this [prescription], I went to the pharmacy to buy this and […] the salesperson told [me] that it was for cancer. And I got scared.
According to the interviewer, the prescription in question was likely to be for vitamins. The incorrect 'expert' knowledge provided by unregulated pharmacies resulted in the respondent being shaken from the experience, explaining that:
since they told me it was cancer, I was shocked […] I couldn't sleep all night because I was so worried.
Although this situation occurred in part due to a lack of communication with the patient's doctor who did not explain the diagnosis or medicine to her, doctors nonetheless feel that pharmacies need stricter regulations to tackle both misinformation and antibiotic resistance:
Doctors mainly have limitations, but […] the drug stores are out of control.
To reduce [antibiotic resistance], the main thing is […] to put strict regulations to the pharmacies. Like only those who received training or those who have a licence can open up pharmacies.
Tackling antibiotic resistance with stricter enforcement of regulation could also reduce the diffusion of false information that is potentially understood by patients as 'expert' knowledge.
The objective of this paper was to investigate the factors that drive the differences in 'lay' and 'expert' medical knowledge in the context of fever treatment in Yangon, Myanmar. Findings of this study show that the level of education of patients, the collective knowledge of the community that can be tied to familial knowledge, and the knowledge contributed by unregulated pharmacies are the key factors that enable differences between 'lay' and 'expert' medical knowledge.
Broadly, the capability approach illustrates that following the generally good access to healthcare providers and medicines in Yangon, several conversion factors define how each individual chooses to be treated for a fever, as well as change the way healthcare providers work to deliver treatment and medicine. Conversion factors are the context-specific reasons as to why the fever treatment and the outcomes of treatment can differ from patient to patient and healthcare worker to healthcare worker. These factors are individual (the age and education of patients), social (socially rooted/familial knowledge as well as the Burmese culture of arriving early to clinics), institutional (the lack of pharmacy regulation and understaffing of healthcare workers), environmental (variations in demand for health services due to seasonality and occurrence of natural disasters) and technological (the types and variety of tests offered by clinics) in nature. The list of possible actions or states that the patient has the freedom to choose to work towards achieving is the capability set. Having good health ensures that patients can choose to achieve what Nussbaum, adapted by Ariana and Naveed (2009), defines as the fundamental aspects of a good life (high life expectancy; bodily health capability; bodily integrity/the ability of the body to move freely; senses, imagination and thought; a lack of affiliation to an illness that can affect an individual's sense of self; and play/participation in recreational activities). The results of this study show that patients felt being relieved from fever symptoms and being healthy enough to work are the desired outcomes of treatment and what they value in life (functionings). The journey towards achieving functionings can involve the exercising of agency. This can be achieved through communicating 'lay' knowledge with doctors, which can then enable a move beyond typical paternalistic doctor–patient relationships.
The social research of this study is helpful for highlighting what 'lay' knowledge can offer to understandings of health, as well as the complex interactions existing between 'lay' and 'expert' knowledge. Therefore, this study contributes to the growing literature on the qualitative experiences of healthcare workers and patients to illustrate their importance in informing public policy.
A limitation to this research, however, is possible construction bias, as highlighted by Robeyns (2006). Using secondary data that was not collected with the intention of inputting into the CAF means these findings are not derived from an optimal dataset. To rectify this for future research, collecting data created for the inputting to the CAF would lead to more reliable results.
Additionally, as the nature of the capability approach is 'radically underspecified' (Robeyns, 2006: 371), the adaptation of the capability approach is highly individual and open to interpretation – to the extent that even when reproduced using the same data, another researcher may find completely different results. This raises the question of how useful such a framework is for real-world application – in the field of policymaking, for example – if outcomes of a study are highly dependent on the researcher and researcher's background. However, if in future research, researchers from multiple backgrounds interpreted the same dataset, an aggregated form of the capability approach could be constructed to fulfil the multi-disciplinary nature of the framework.
This research highlights the usefulness of communication with healthcare workers and patients to understand their interactions with health in their own words. Factors such as the education of patients, the pool of collective 'lay' knowledge and institutional context must be considered by policymakers when designing biomedical health policies and interventions. Although unintended consequences are inevitable, considering such factors can improve the likeliness of successful health intervention and policies.
Further research in the form of an ethnography could be undertaken to investigate the variations of knowledge across Myanmar. Observing the behaviour described by respondents in their interviews and focus groups, as well as collecting data from a number of regions and for a greater variety of illnesses, would allow a more comprehensive understanding of Myanmar's health system on a national scale. Furthermore, data should be collected from both males and females as, although only data from female participants was provided by Haenssgen et al. (2019), studying how both sexes interact with their local environments and knowledge bases would provide a more accurate overview of Myanmar's health system.
I wish to express my gratitude to Dr Marco J. Haenssgen (Global Sustainable Development, University of Warwick) for his supervision and support on this paper. Additionally, I extend my thanks to Marco J. Haenssgen; Thomas Althaus and Yoel Lubell (Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, University of Oxford); Nutcha Charoenboon and Yuzana Khine Zaw (Mahidol Oxford Tropical Medicine Research Unit); Nga T. T. Do and Heiman F. L. Wertheim (Oxford University Clinical Research Unit (OUCRU)) for allowing the use of their Myanmar data sub-set in this research paper. Furthermore, thank you to the editorial team at Reinvention and the two anonymous peer reviewers for their helpful comments.
Figure 1: Map of Myanmar, source: Wikimedia Commons, 2009.
Figure 2: Basic outline of the CAF; diagram constructed by author, adapted from Alkire and Deneulin, 2009; Haenssgen, 2020; Haenssgen and Ariana, 2017; Robeyns, 2005.
Figure 3: An illustration of the capability approach adapted to the case of fever treatment in Yangon, Myanmar. Diagram constructed by the author, adapted from Alkire and Deneulin, 2009; Ariana and Naveed, 2009; Haenssgen, 2020; Haenssgen and Ariana, 2017; Robeyns, 2005.
Table 1: Table illustrating the characteristics of the study population for both the SSIs and FGDs.
[1] Wellcome Trust Institutional Strategic Support Fund, ref. 105605/Z/14/Z; ClinicalTrials.gov Identifier NCT02758821; Principal Investigator: Dr Yoel Lubell.
[2] Ref. 49–15
[3] Ref. Ethics/DMR/2016/137
Alkire, S. and S. Deneulin (2009), 'Part I: Concepts: The human development and capability approach', in Deneulin, S. and Shahani, L. (eds), An Introduction to the Human Development and Capability Approach: Freedom and Agency, London: Earthscan Publications, pp. 22–48
Ariana, P. and A. Naveed (2009), 'Part II: Topics: Health', in Deneulin, S. and Shahani, L. (eds), An Introduction to the Human Development and Capability Approach: Freedom and Agency, London: Earthscan Publications, pp. 228–45
Bury, M. (2001), 'Illness narratives: fact or fiction?', Sociology of Health & Illness, 23 (3), 263–85
Coderey, C. (2021), 'Myanmar traditional medicine: The making of a national heritage', Modern Asian Studies, 55 (2), 514–51, available at https://doi.org/10.1017/S0026749X19000283, accessed 9 April 2021
Fusch, P. and L. Ness (2015), 'Are we there yet? Data saturation in qualitative research', The Qualitative Report, 20 (9), 1408–16, available at https://doi.org/10.46743/2160-3715/2015.2281, accessed 10 April 2021
Given, L., (ed.) (2012), 'Data saturation', in The SAGE Encyclopedia of Qualitative Research Methods, Thousand Oaks: SAGE Publications, pp. 196
Goodyear-Smith, F. and S. Buetow (2001), 'Power issues in the doctor-patient relationship', Health Care Analysis, 9, 449–62
Haenssgen, M. J. (2020), Interdisciplinary Qualitative Research in Global Development, Bingley: Emerald Publishing Limited
Haenssgen, M. J. and P. Ariana (2017), 'The place of technology in the capability approach', Oxford Development Studies, 46 (1), 98–112, available at https://doi.org/10.1080/13600818.2017.1325456, accessed 22 April 2021
Haenssgen, M. J., N. Charoenboon, N. D. T. Thuy, T. Althaus, Y. K. Zaw, H. F. L. Wertheim and Y. Lubell (2019), 'How context can impact clinical trials: A multi-country qualitative case study comparison of diagnostic biomarker test interventions', Trials, (20) 111, available at https://doi.org/10.1186/s13063-019-3215-9, accessed 22 April 2021 (Myanmar data subset, provided with permission)
Khaing, I., A. Malik and N. Hamajima (2015), 'Health care expenditure of households in Magway, Myanmar', Nagoya Journal of Medical Science, 77 (1–2), 203–12
Lambert, H., M. Chen and C. Cabral (2019), 'Antimicrobial resistance, inflammatory responses: A comparative analysis of pathogenicities, knowledge hybrids and the semantics of antibiotic use', Palgrave Communications, 5 (1), available at https://doi.org/10.1057/s41599-019-0293-y, accessed 8 April 2021
Lwin, M., M. Sudhinaraset, A. San and T. Aung (2014), 'Improving malaria knowledge and practices in rural Myanmar through a village health worker intervention: A cross-sectional study', Malaria Journal, 13 (1)
McClean, S. and A. Shaw (2005), 'From schism to continuum? The problematic relationship between expert and lay knowledge—an exploratory conceptual synthesis of two qualitative studies', Qualitative Health Research, 15 (6), 729–49
Moes, F., E. Houwaart, D. Delnoij and K. Horstman (2020), 'Questions regarding 'epistemic injustice' in knowledge-intensive policymaking: Two examples from Dutch health insurance policy', Social Science & Medicine, 245, 11 (2674), available at https://doi.org/10.1016/j.socscimed.2019.112674, accessed 8 April 2021
Oxford English Dictionary (2020), 'biomedicine, n.', Oxford English Dictionary, Oxford: Oxford University Press
Peltzer, K., W. Oo and S. Pengpid (2016), 'Traditional, complementary and alternative medicine use of chronic disease patients in a community population in Myanmar', African Journal of Traditional, Complementary and Alternative Medicines, 13 (3), 150–55
Prior, L. (2003), 'Belief, knowledge and expertise: The emergence of the lay expert in medical sociology', Sociology of Health & Illness, 25, 41–57
Risso-Gill, I., M. McKee, R. Coker, P. Piot and H. Legido-Quigley (2013), 'Health system strengthening in Myanmar during political reforms: Perspectives from international agencies', Health Policy and Planning, 29 (4), 466–74
Robeyns, I. (2005), 'The capability approach: A theoretical survey', Journal of Human Development, 6 (1), 93–117, available at https://doi.org/10.1080/146498805200034266, accessed 8 April 2021
Robeyns, I. (2006), 'The capability approach in practice', The Journal of Political Philosophy, 14 (3), 351–76
Sein, T. T., P. Myint, N. Tin, H. Win, S. Aye and T. Sein (2014), 'The Republic of the Union of Myanmar health system review', Health Systems in Transition, 4 (3)
Sommanustweechai, A., W. Putthasri, M. Nwe, S. Aung, M. Theint, V. Tangcharoensathien and S. Wynn (2016), 'Community health worker in hard-to-reach rural areas of Myanmar: Filling primary health care service gaps', Human Resources for Health, 14 (1)
Thu, A., H. Win, M. Nyunt and T. Lwin (2012), 'Knowledge, attitudes and practice concerning tuberculosis in a growing industrialised area in Myanmar', The International Journal of Tuberculosis and Lung Disease, 16 (3)
Wikimedia Commons (2009), 'Map of Myanmar with regions colour coded', available at https://commons.wikimedia.org/wiki/File:Burma_Regions_Map.png, accessed 27 November 2020
Wiseman, N. (2004), 'Designations of medicines', Evidence-Based Complementary and Alternative Medicine, 1 (3), 327–29
Zaw, P., T. Htoo, N. Pham and K. Eggleston (2015), 'Disparities in health and health care in Myanmar', The Lancet, 386, (2053)
Zaw, Y., N. Charoenboon, M. Haenssgen and Y. Lubell (2018), 'A comparison of patients' local conceptions of illness and medicines in the context of C-reactive protein biomarker testing in Chiang Rai and Yangon', The American Journal of Tropical Medicine and Hygiene, 98 (6), 1661–70, available at https://doi.org/10.4269/ajtmh.17-0906, accessed 10 April 2021
To cite this paper please use the following details: Hoque Syed, O. (2021), 'Investigating the factors behind differences in 'lay' and 'expert' medical knowledge in the context of fever treatment in Yangon, Myanmar', Reinvention: an International Journal of Undergraduate Research, Volume 14, Issue 1, https://reinventionjournal.org/article/view/732. Date accessed [insert date]. If you cite this article or use it in any teaching or other related activities please let us know by e-mailing us at Reinventionjournal@warwick.ac.uk.