Rebecca Kirkham and Caitlin Batten, Monash University
New technologies such as virtual reality (VR) and mobile apps are increasingly being developed and trialled therapeutically to help treat anxiety disorders. Despite this increasing market, there is little research on how the public perceive the incorporation of these innovative technologies in anxiety treatment. This study aimed to describe knowledge, awareness and perceptions of VR and mobile apps for the treatment of anxiety. To do this, a survey was disseminated to those aged 18 to 35 with no current or previous mental illness via social media and poster advertisements, and 57 individuals participated. Results demonstrated that most individuals had limited knowledge on the use of VR and mobile apps in mental health, but overall demonstrated positive perceptions and high optimism regarding its potential use. Neither treatment modality was perceived as being as effective as standard treatment; however, participants were willing to use either modality if recommended by a therapist and use both in conjunction with standard treatment. Participants demonstrated a willingness to use a mobile app as a first point of contact. These findings have implications for the way in which these technologies are rolled out to the public.
Keywords: Virtual reality, VR, mobile apps, anxiety treatment, mental health treatment, public perceptions
In 2018, around 4.8 million people in Australia (20 per cent of the population) lived with a mental health condition (Australian Bureau of Statistics (ABS), 2018). In the space of three years between 2015 and 2018, this prevalence had increased by 800,000 people (2.6 per cent of the population), predominantly driven by an 11 per cent rise in anxiety-related disorders – which alone affect 13 per cent of all Australians (ABS, 2018). Those most affected are aged between 18 and 35, when anxiety onset is most common (Lijster et al., 2017). These conditions have a detrimental impact on an individual’s quality of life, family and community dynamics, and contribute to both the direct and indirect productivity loss amounting to $56.7 billion annually (The Royal Australian and New Zealand College of Psychiatrists (RANZCP), 2014). Given this extensive and increasing burden, effective treatment options and preventative measures are crucial.
Treatment for anxiety is predominantly one of two types: psychotherapy or pharmaceuticals. One type of psychotherapy, cognitive behavioural therapy (CBT), has significant research support and is currently the ‘gold standard’ (David et al., 2018) first-line treatment for anxiety (Arch and Craske, 2009). However, meta-analyses and systematic reviews have identified that response rates to CBT for anxiety disorders are as low as 50 per cent (Hofmann et al., 2012; Loerinc et al., 2015). As an alternative to psychotherapy, pharmaceuticals (Donker et al., 2013) are increasingly used and widely available (Farach et al., 2012). However, pharmaceutical response rates are estimated to be only 50–60 per cent, and critically, remission rates are as low as 25–35 per cent (Bystritsky, 2006; Roy‐Byrne, 2015). Further, pharmacotherapy is often an insufficient treatment alone (Taylor et al., 2012) and an adjunctive therapy, such as CBT, is often required. Additionally, Australian anxiety sufferers encounter significant barriers to seeking treatment in the first place resulting in up to 73 per cent of those with anxiety symptoms not seeking treatment at all (Harris et al., 2015). One contributor to this is low mental-health literacy, which is a limited ability to recognise and label one’s symptoms and beliefs around the progression of symptoms (Jorm, 2000). Low mental-health literacy contributes to a lack of treatment-seeking through misattribution and mislabelling of symptoms and unawareness of the treatment options, suitability and outcomes (Coles and Coleman, 2010). Additionally, both the stigma one perceives from others via societal rejection due to behaviour, appearance or mental illness (Curcio and Corboy, 2020) and internalised self-stigma whereby the individual labels themselves as being unacceptable for experiencing anxiety difficulties (Vogel et al., 2006) additively contribute to a lack of help-seeking (Vogel et al., 2007). Finally, other barriers such as cost impede treatment-seeking, particularly for the proportion of those with comorbid physical or mental illness, or other medical problems (RANZCP, 2015). Thus, there is substantial room for improvement to increase the accessibility of treatments for anxiety sufferers and improve their effectiveness. This is imperative to address in order to reduce the significant burden anxiety disorders create for individuals and society at large.
Recent developments in virtual reality (VR) technology and increased access to technology such as smartphones are shifting how anxiety disorders are treated (Valmaggia et al. 2016). VR and mobile apps are being developed and trialled to treat mental illness (Anderson et al., 2003, Lipschitz et al., 2019). These technological advancements inspire new opportunities for alternative, more accessible and effective treatment platforms. Specifically, VR is often trialled in anxiety disorders (Carl et al., 2019) including, but not limited to, social anxiety disorder (Kampmann et al., 2016) and specific phobias (Cote and Bouchard, 2008). An example of this is VR exposure therapy, whereby the client engages with VR technology and its virtual environment to be systematically introduced to the feared stimulus with the guidance of a mental health professional (Parsons and Rizzo, 2008). Supporting VR’s effectiveness, a meta-analysis and systematic review support the use of VR in exposure therapy (Botella et al., 2017), showing large effect sizes compared to control conditions and no difference to the standard modality of in-vivo exposure therapy (Carl et al., 2019). Critically, the therapy conducted within the virtual environment has been shown to generalise to real-life contexts, demonstrating its ecological validity (Morina et al., 2015). One of the significant advantages to VR exposure therapy is that the therapist may elicit exposure to stimuli that would otherwise be unable to be mimicked within the therapist’s office (Bouchard et al., 2017). Further, acceptability of exposure therapy is greater for VR modalities than in-vivo (Garcia-Palacios et al., 2007). Partnered with the increasing accessibility (Bouchard et al., 2017), VR reduces issues in accessing and receiving treatment.
Additionally, there are a plethora of mobile apps on the market targeting disorders such as social anxiety (Alyami et al., 2017), general anxiety disorder and others (Sucala et al., 2017). For example, a mobile app targeting social anxiety disorder may take users through a self-help programme structured into modules that each address various challenges and encourage completion of exercises (Stolz et al., 2018). In turn, the mobile app can provide motivational enhancement, guide the user through behavioural experiments and provide relapse prevention strategies for maintaining the skills learnt (Stolz et al., 2018). Despite the estimate that less than 5 per cent of mobile apps on available are rigorously tested (Sucala et al., 2017), a meta-analysis of randomised control trials for anxiety smartphone interventions revealed that these interventions evoke a significantly greater reduction in anxiety symptoms compared to control conditions (Firth et al., 2017). This suggests that when rigorously tested, mobile apps provide another technological platform of therapy with which anxiety sufferers can engage. Additionally, the pairing of VR and the mobile app platform has successfully delivered a treatment for phobias without therapist intervention in a randomised clinical trial (Donker et al., 2019), further demonstrating the potential of these two modalities in both independent and integrated formats.
Developments in the capabilities of VR and mobile apps open the door to new forms of evidence-based treatment that is more accessible and affordable than other standard treatments. However, while these new technologies have incredible potential, it is unclear how potential users perceive these new modalities of therapy, particularly VR. One study conducted by Keller and colleagues (2017) used Facebook comment content analysis on a video demonstrating VR therapy to gauge the public’s perception of VR use within the healthcare sector. Three-quarters of comments (n = 1614, 74.16 per cent) expressed positive perceptions about VR use within the healthcare sector, with 15.56 per cent expressing negative views and 34.70 per cent giving ‘neutral’ views. Some comments expressed mixed or multiple perceptions. This suggests that those who already engage with technological platforms, such as social media, are optimistic about VR’s inclusion in the healthcare sector. However, it is unclear whether firstly, this extends to mental health, secondly, whether this is true for anxiety-related problems and thirdly, whether this is true for 18- to 35-year-olds who are at higher risk of developing an anxiety-related problem (Lijster et al., 2017). If such individuals have limited knowledge or negative perceptions towards treatment, they are less likely to obtain help (Reardon et al., 2017) in the early stages of the illness where intervention is thought to reduce prevalence of developing an anxiety disorder (Osuch et al., 2015, Topper et al., 2017). In conjunction with assuring the effectiveness of these technological treatment modalities themselves, understanding how this age group perceive such modalities is critical to ensure effective implementation into mental healthcare if these individuals do begin to suffer anxiety problems. The aim of this exploratory survey was to describe knowledge, awareness and perceptions of VR and mobile apps for the treatment of anxiety among a sample of 18- to 35-year-olds with no current or previous mental illness. Specifically, for VR and mobile apps uniquely, this study sought to, 1) determine perceived level of effectiveness, 2) determine perceived legitimacy, 3) evaluate respondents’ willingness to engage and 4) understand the perceived comparison to common treatment methods. This research provides insights into how to successfully roll out novel technological platforms for anxiety treatment.
To be included within the study, participants had to be aged between 18 and 35 and have no current or previous diagnosis of a mental health disorder. Participants were recruited via advertisements on both the campus and online within the Monash University community and social media advertisements to the general community. The survey was completed on an online Google Forms survey platform.
The study was approved by the Monash University Human Research Ethics Committee (See Appendix B for Ethical Approval Notice).
The survey was distributed via social media platforms such as Facebook as well as on a QR code on flyers that were posted around the Monash University Clayton Campus. These methods were chosen to best target the eligible demographic of those aged 18–35. The survey was active for 14 weeks from 8 March 2019 to the 18 June 2019.
The survey asked participants to first read the explanatory statement that explained what was involved in the survey, information about confidentiality, possible benefits and risks, and included links and numbers to mental health helplines for participants who experienced any discomfort.
The survey comprised of 3 demographic questions, 2 eligibility questions, 6 multiple-choice questions and 19 Likert-scale questions. These questions were formulated based on the results from preliminary research papers on public perceptions of VR in healthcare (Keller et al., 2017).
The multiple-choice questions assessed participants’ current knowledge of the role of VR and mobile apps in the mental health sector. Participants were then presented with a short paragraph of information on the current use of VR and mobile apps in mental health to aid with the next Likert-scale question section. The following sections asked questions regarding the participants’ willingness to use these technologies, their perceptions on the effectiveness and legitimacy of these technologies and their perceived barriers and advantages to using such technologies. At the conclusion of the survey, participants were thanked for their time.
Survey responses were analysed using Statistical Package for Social Sciences (SPSS) version 25.0. Data was analysed by running descriptive statistics (frequencies, mean) and inferential statistics to examine relationships between responses. A maximum likelihood ratio Chi-square test (McHugh, 2013) was generated for those who have and have not experienced anxiety symptoms as well as those who are and are not aware of the use of VR and mobile apps in healthcare against perceptions of effectiveness and legitimacy for both VR and mobile apps. Cramer’s V indicated the effect size for any significant relationships.
Respondents were asked three main streams of questions on their perception of VR and mobile apps. These were their legitimacy (that is, their validity as treatment tools), their efficacy and their personal willingness to use such tools. Results broadly demonstrated that individuals tended to be aware that mobile apps and, to a lesser extent, VR are used in healthcare. On a five-point Likert scale, a majority of respondents reported that they perceived VR as being moderately illegitimate, and mobile apps as moderately legitimate. Both VR and mobile apps were seen as moderately effective. Of interest, most participants were optimistic and willing to use the platforms; however, they were more willing to use each technology if recommended by a therapist. Finally, individuals indicated that they would be more likely to engage with either platform in conjunction with medication or psychological therapy as opposed to either platform alone.
Please refer to Appendix A for raw survey output.
Participants included 57 individuals (female = 38, male = 19), aged from 18 to 35 (mean = 22). Of these participants, 65 per cent reported having experienced anxiety symptoms at some time in their life since the age of 18 years old, but not having had a diagnosed mental health disorder.
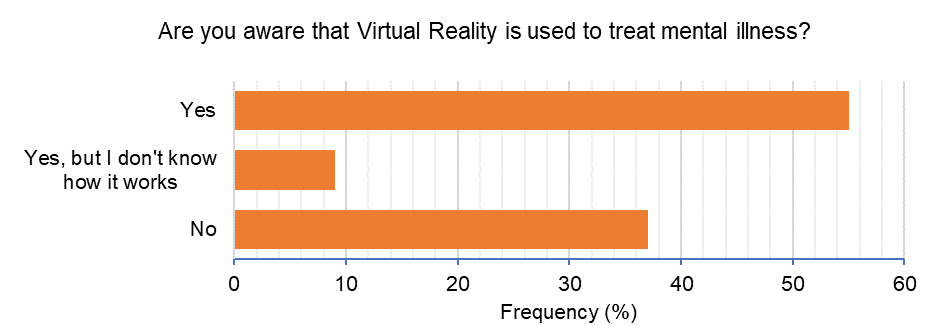
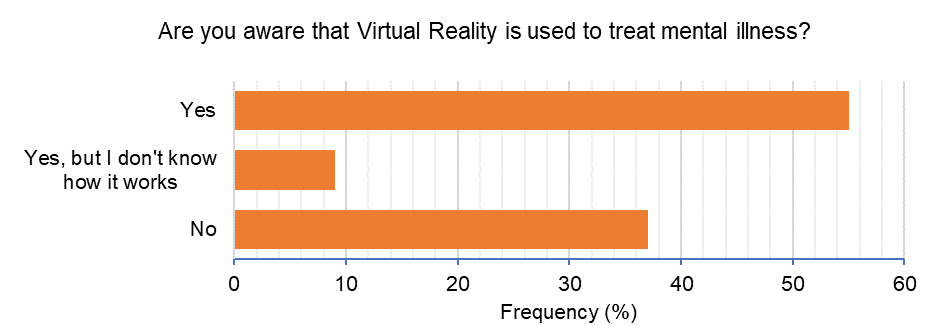
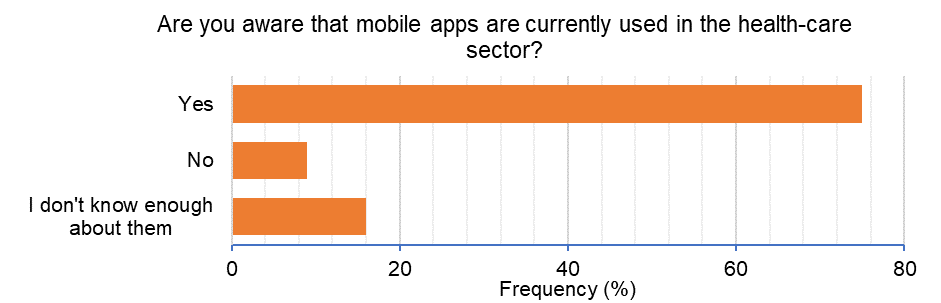
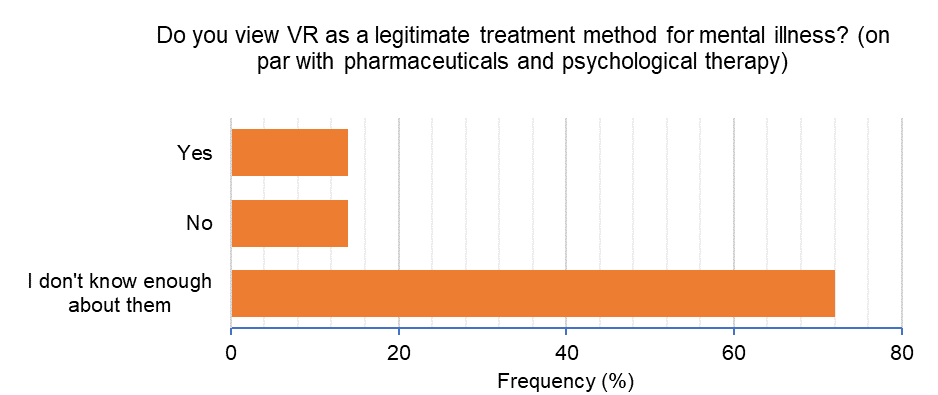
Participants’ current knowledge about VR and mobile apps were assessed prior to any information about the mediums being provided. Responses are detailed in Figures 1a, 1b and 1c.
Additionally, 97 per cent of participants stated that they were interested in the potential uses of technology to help treat mental illness.
Almost three-quarters (72 per cent) of participants reported that they would want to try VR to treat anxiety and anxiety-related mental illness; 23 per cent felt that they do not know enough about it to respond otherwise. An 86 per cent majority responded that they would suggest or inform someone they knew about VR or mobile apps if that person had anxiety symptoms.
Questions for the following sections were answered on a Likert scale ranging from a rating of 1 to 6 with response meanings described in the legend. Negative perceptions are broadly captured in responses from 1 to 3, and positive perceptions from 4 to 6.
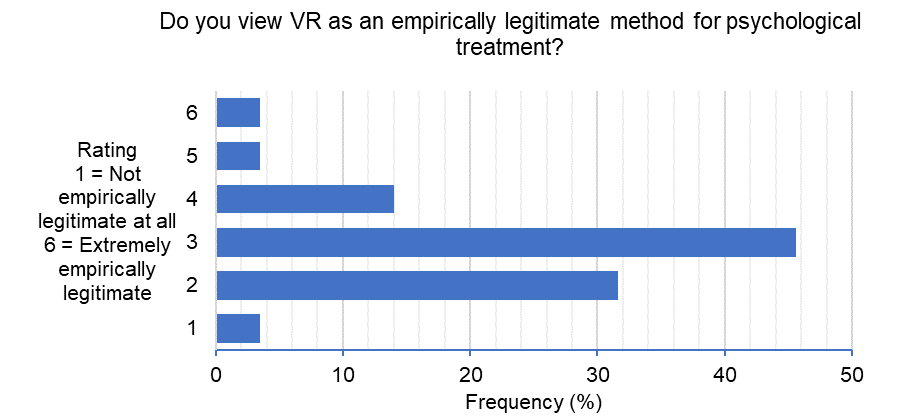
Perceptions about the legitimacy of VR
Figure 2 shows participant perceptions about the legitimacy of VR for psychological treatment for anxiety.
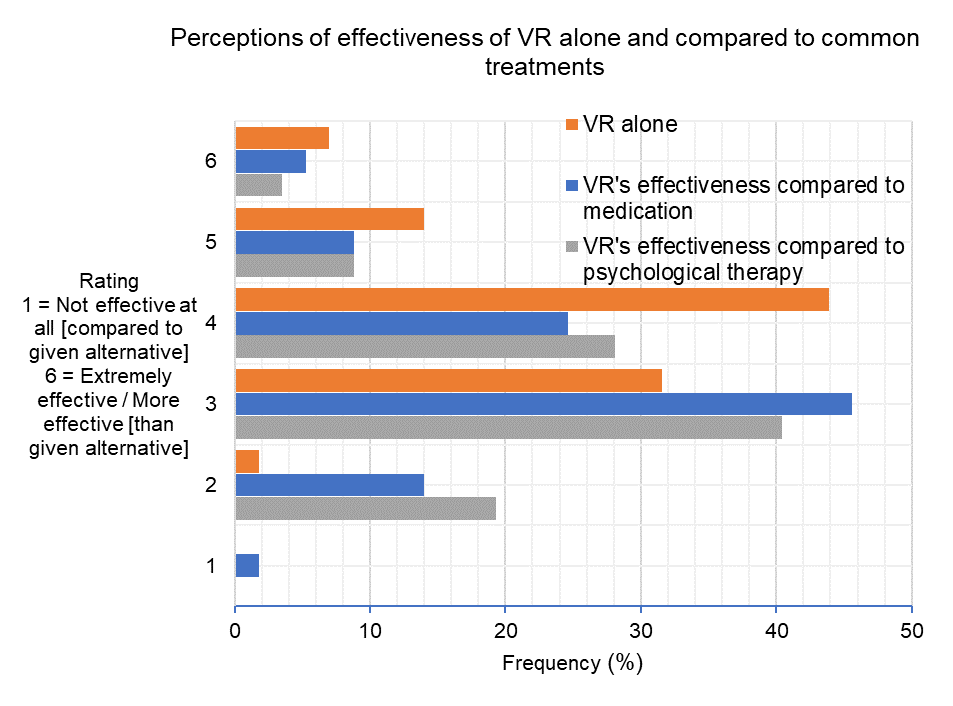
Perceptions of the effectiveness of VR
Figure 3 demonstrates participant’s perceptions on the effectiveness of VR alone, and in comparison to medication and to psychotherapy.
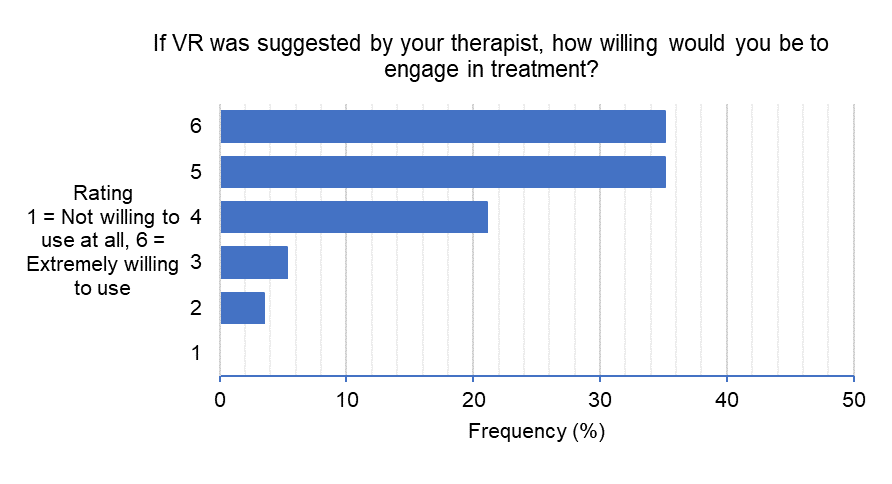
Willingness to use VR
Participants rated that they would be extremely willing to use VR if it was suggested by their therapist, with 91.3 per cent of responses ranging from 4, ‘Moderately willing to use’ to 6, ‘Extremely willing to use’ (Figure 4a).
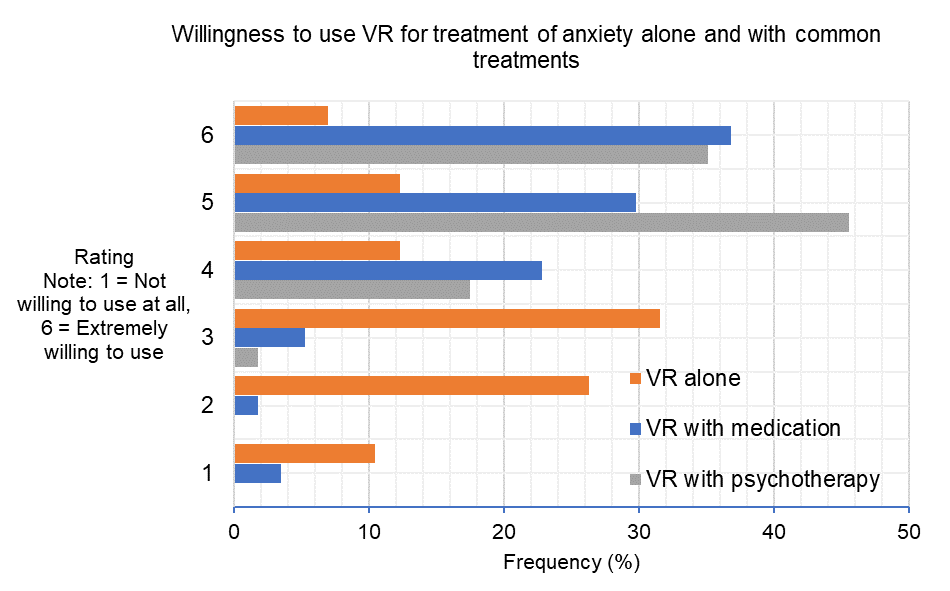
Figure 4b illustrates participants’ ratings of their willingness to use VR as a sole method of treatment for anxiety symptoms, in combination with medication and/or psychotherapy.
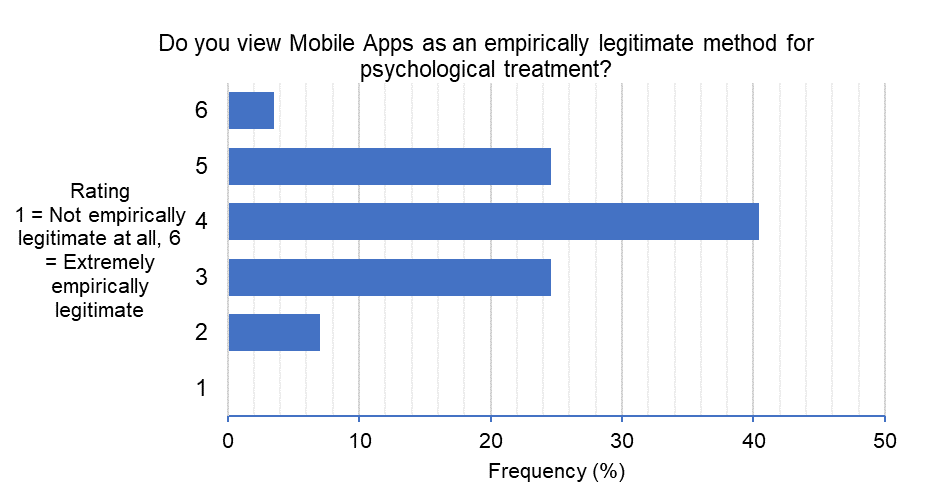
Perceptions about the legitimacy of mobile apps
Most participants viewed mobile apps as being a moderately legitimate method for psychological treatment, with 68.5 per cent of responses in the positive range (Figure 5).
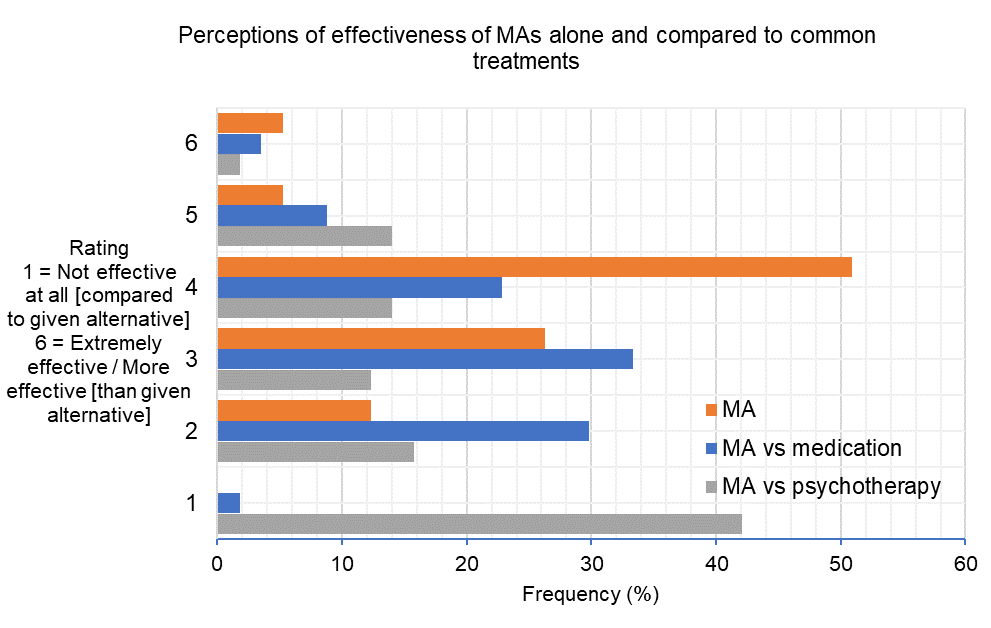
Perceptions about the effectiveness of mobile apps
Figure 6 shows participant ratings on each question pertaining to the effectiveness of mobile apps. A 60.9 per cent majority of participants positively rated the effectiveness of mobile apps. Comparatively, most participants rated mobile apps as less effective than medication (64.9 per cent) and psychotherapy (70.2 per cent).
Willingness to use mobile apps
A majority of participants (84.2 per cent) positively responded that they would be willing to use mobile apps if suggested by their therapist (Figure 7a). A slight majority of participants responded that they would be willing to use mobile apps as their first point of contact over a medical practitioner or psychological therapist for help (Figure 7b). Figure 7c illustrates participants’ ratings on willingness to use mobile apps alone and in conjunction with medication and psychological therapy. A slight majority (56.1 per cent) responded in the negative range that they would not be willing to use mobile apps as a sole method of anxiety treatment. Comparatively, 82.5 per cent and 87.8 per cent of responses were positive for using mobile apps in conjunction with medication and psychotherapy, respectively.
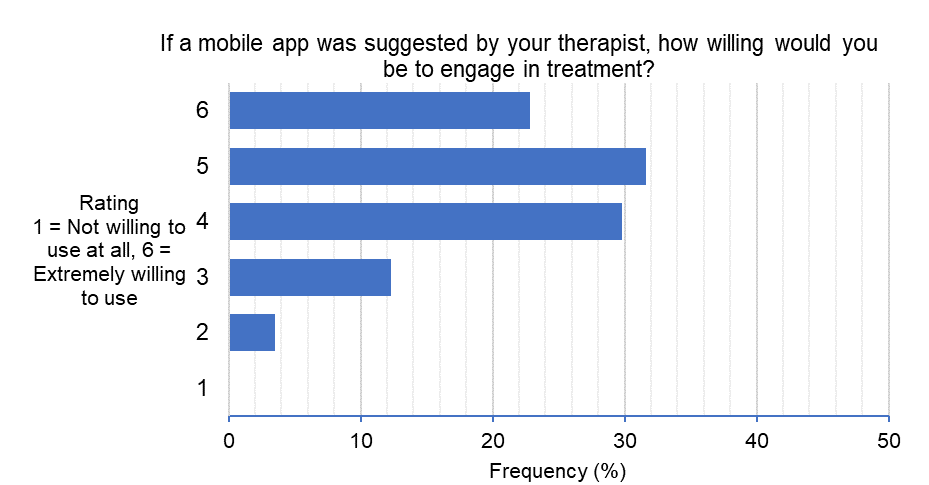
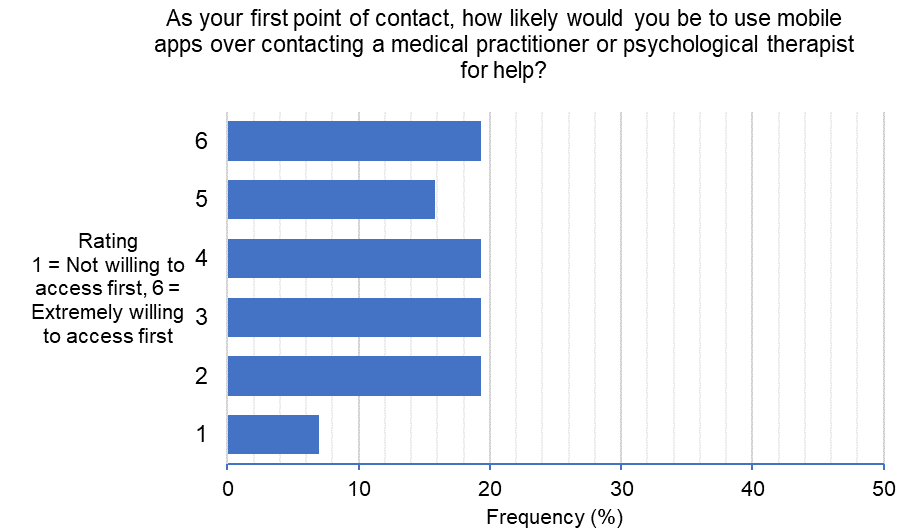
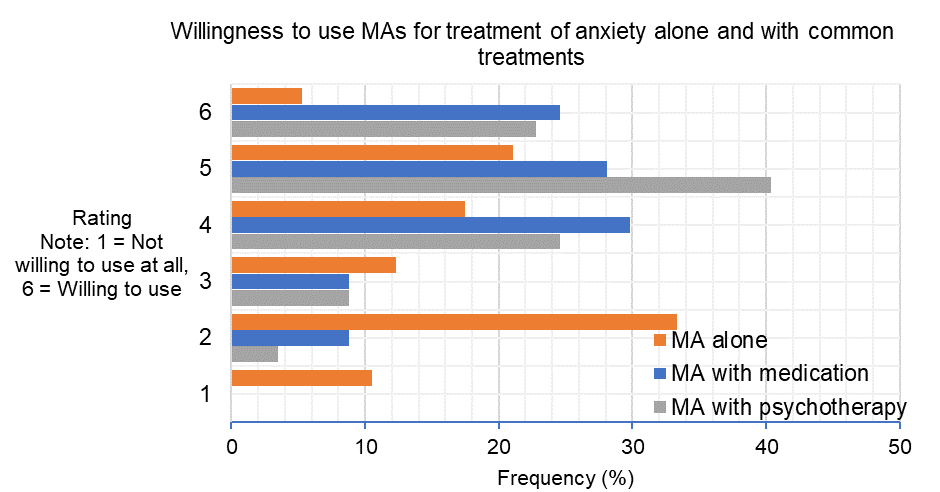
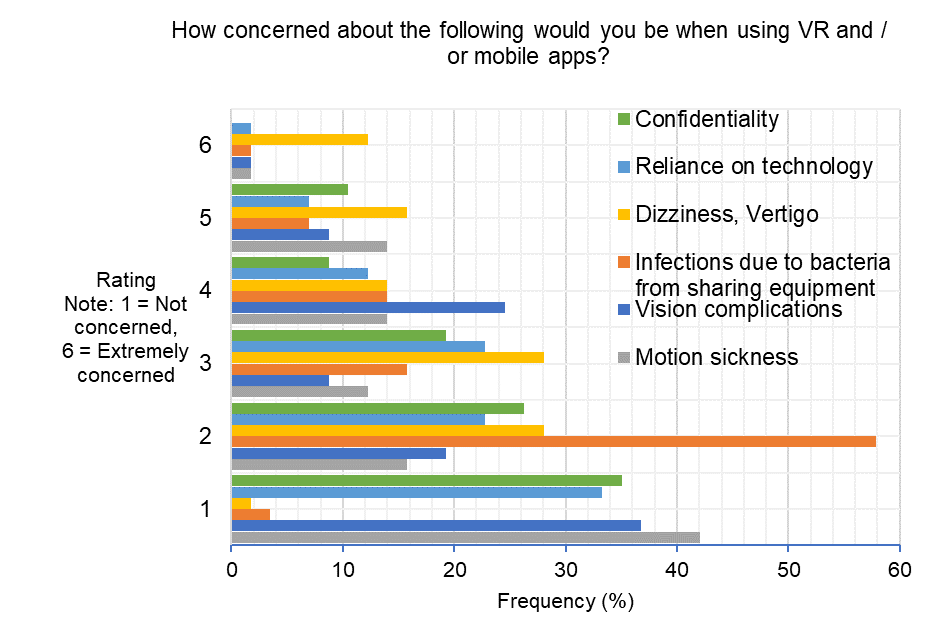
Figure 8 illustrates participants’ perceptions on a range of potential barriers to using VR and mobile apps including confidentiality, reliance on technology, dizziness/vertigo, infections due to bacteria from sharing equipment, vision complications and motion sickness.
A maximum likelihood ratio Chi-square test revealed a significant relationship between having experienced anxiety symptoms and perceptions of VRs effectiveness for anxiety (χ2 (4) = 26.67, p <.00) with a ‘large’ effect size, Cramer’s V (1, N = 55) =.61, p <.00 (Cohen, 1988). On further inspection, this was largely driven by a greater negative rating of VR’s effectiveness by the anxiety-experienced group. There were no other significant relationships between having experienced anxiety symptoms and perceived effectiveness of mobile apps (χ2 (8) = 8.80, p =.40), legitimacy of VR (χ2 (4) = 8.21, p =.10), or mobile apps (χ2 (8) = 8.33, p =.46), or likelihood of using a mobile app as first point of contact in seeking help for anxiety (χ2 (5) = 6.05, p =.37).
Additionally, there were no significant relationships between knowledge that VR is used in mental healthcare and perceptions of its effectiveness (χ2 (8) = 6.74, p =.64) or legitimacy (χ2 (8) = 7.99, p =.50). Nor any significant relationship between knowledge that mobile apps are used in the healthcare sector and perceptions of their effectiveness (χ2 (8) = 8.80, p =.40) or legitimacy (χ2 (8) = 8.83, p =.46).
This study on VR and mobile app technology used a convenience sample of 18- to 35-year-olds without current or previous mental illness to survey their knowledge, awareness and perceptions of using such technologies for anxiety treatment. The online survey generated several key findings.
Regarding current knowledge (Figures 1a–1c), half of the sample did not know that VR was currently being used in mental health treatment. This is unsurprising given the non-clinical sample and scarce implementation of VR across mental health locations. Contrastingly, however, three-quarters were aware that mobile apps were used in the healthcare sector. Broadly, the healthcare sector includes general practitioner services, which are frequented more than mental healthcare service (ABS, 2015), and mobile apps are more prevalent across these locations and serve a variety of functions (Overdijkink et al., 2018; Postolache et al., 2014; Postolache et al., 2015). This contrasts significantly with VR, which is not used widely with the public. In a similar vein, nearly three-quarters of participants indicated that they did not know enough about VR to assess whether it was a legitimate treatment method. This is likely due to the lack of contact and knowledge surrounding VR and highlights the need for education surrounding the service when it is introduced to a new client, perhaps more so than the use of a mobile app. Despite this lack of exposure, all bar two participants responded that they were interested in technology in mental health treatment. This overwhelming interest in this space indicates that education and the use of VR and mobile apps in therapy is likely to be well received. This result is also encouraging for treatment adherence to a VR or mobile app therapy.
In line with past research, this study found positive public perceptions towards VR (Keller et al., 2017). However, overall, participants viewed VR as moderately illegitimate (Figure 2a) and moderately effective (Figure 3), demonstrating a sense of uncertainty. This uncertainty, however, was overcome by the recommendation to engage with VR if suggested by a therapist (Figure 4a), whereby an overwhelming majority (91.3 per cent) showed a willingness to engage. This highlights the importance of treatment expectations, which may significantly alter not only the willingness to engage in therapy, but the outcomes of therapy and the therapeutic relationship (Wampold, 2015). Of interest, those who stated that they had experienced anxiety symptoms perceived that VR was less effective compared to those who said they had not experienced anxiety symptoms. This result appears to be driven by the anxiety-experienced group perceiving VR as less effective than their non-experienced counterparts.
The differing response pattern between anxiety-experienced and non-experienced respondents on the effectiveness of VR is similar to the response pattern for perceived legitimacy of VR, although this difference was not statistically significantly different. Nonetheless, the pattern whereby anxiety-experienced individuals rate the legitimacy and effectiveness of VR as less than their non-experienced counterparts could be interpreted as an increased uncertainty that VR could be a valid and effective treatment tool. The lack of personal reference for the non-experienced group may mean that they are less able to conceive the problems VR would need to address as a therapy, and thus rate VR more optimistically than their experienced counterparts. To bolster the effectiveness of VR in therapy, clients should be provided information surrounding the effectiveness and legitimacy of this technology prior to, or early in, the therapy process, since client expectations affect therapy outcomes (Field et al., 2017; Greenberg et al., 2006).
Overall, participants indicated that they would be more willing to use VR if their therapist suggested it, or in conjunction with another treatment for anxiety such as medication, rather than using VR as a standalone treatment, which further indicates the participants’ uncertainty around the platform (Figure 4b). Concurrently, this demonstrates a consistency between public perceptions and the current state of the literature, where it is suggested that more rigorous research must be conducted before VR can be a standalone therapy (Zeng et al., 2018).
Mobile apps, however, were viewed as being moderately effective (Figure 6) and moderately legitimate (Figure 5a). This is in line with previous responses, indicating that the present sample have more exposure to, and knowledge about, mobile apps used in healthcare sectors. This greater exposure to mobile apps over VR may have contributed to higher ratings of perceived legitimacy. Furthermore, participants were highly likely to engage with a mobile app if recommended by their therapist (Figure 7a), but were generally less willing to use it as a sole treatment method, preferring the mobile app to be used in conjunction with another therapy (Figure 7c). This reflects what is currently seen in healthcare, where apps are commonly used as an additive tool to standard treatment (Overdijkink et al., 2018; Postolache et al., 2015).
Participants were asked to compare the effectiveness of VR and mobile apps separately to psychotherapy such as CBT and medication. As illustrated in Figure 3, most participants perceived that VR was somewhat ineffective compared to both psychotherapy and medications. In comparison to standard treatment, participants perceived mobile apps alone to be not as effective as medications for anxiety treatment and not effective at all compared to psychotherapy (Figure 6). Although some studies focusing on the effectiveness of VR compared to standard treatment for anxiety demonstrate promising outcomes, few mobile apps that are released publicly are tested as rigorously with a sufficient evidence base in the same manner (Sucala et al., 2017; Lui et al., 2017.) Despite showing effectiveness when empirically supported, this plethora of unsubstantiated mobile apps available (Wang et al., 2018) likely creates an overall perception of ineffectiveness from respondents towards mobile apps.
The survey additionally asked participants whether they would be likely to use a mobile app as a first point of contact over a medical practitioner or psychological therapist. Figure 7b shows these responses ranging significantly across the scale with almost equal proportions responding from 2 to 6. This is interpreted as an overall positive response, considering that common barriers such as cost and stigma can be reduced by using a mobile app (Coates et al., 2019). Here, our respondents demonstrate a likelihood to use an available mobile app as their first point of contact in getting help. The availability of such a tool could ultimately increase help-seeking behaviour and reduce the prevalence of untreated anxiety problems. Although not specifically explored in this study, this could be particularly instrumental in encouraging and enabling people from minority and marginalised groups who suffer higher rates of anxiety disorders (Nasir et al., 2018; Said et al., 2013) to take the first step in accessing healthcare.
Interestingly, participants’ knowledge of VR and mobile apps being used in the mental health and healthcare sectors respectively was not related to their perceptions of their effectiveness or legitimacy, suggesting that awareness does not equate to opinion in this space. This highlights the importance of education on the effectiveness and legitimacy of VR and mobile apps regardless of whether people are aware of or have been in contact with these modalities previously.
Finally, the survey assessed perceptions on barriers to using VR and mobile apps (Figure 8). Dizziness and vertigo were perceived as the greatest concern; however, this was only for a minority of the sample. Many studies find that there is no increase in these symptoms (generalised as cybersickness) when assessed before and after using immersive VR (Bouchard et al., 2017; Weech et al., 2019). However, this finding remains key for the implementation of VR given that anxiety levels prior to VR immersion may inflate the side-effects from the experience (Bouchard et al., 2009). Given that a small proportion of individuals have concerns about elements of dizziness and vertigo, introducing VR with information and gradual experience may be useful to mitigate some users’ concern.
The current findings should be interpreted within the context of several limitations. Firstly, 57 individuals responded to the survey, predominantly through social media and through on-campus advertisements at Monash University. This sample is small and does not represent the Australian population at large. Thus, our results should be interpreted with caution in applying to a predominantly young-adult, university population. Similarly, we recruited participants without current or previous mental illness. Although many participants have experienced anxiety symptoms, the views of these individuals may be different to those with clinical levels of anxiety. Nonetheless, the views of those with sub-clinical thresholds of anxiety in the 18- to 35-year-old age group remain critically important to understand, given that they are still at greatest risk of experiencing an anxiety condition during these years. If such individuals have limited knowledge or negative perceptions towards treatment, they are less likely to obtain help in the early stages of the illness where intervention is critical and most effective. Given that this study’s aim was to assess the public’s perceptions of using VR and mobile apps in anxiety treatment, participants were not provided with extensive information on how VR and mobile apps may be incorporated into treatment, nor the capacity in which they are used.
Additionally, the survey did not explain what psychotherapy or CBT entailed or the types of medications used in anxiety treatment. This is concurrently a strength and weakness of the study. While we captured participants’ raw perceptions with their current knowledge, participants could not provide an informed opinion on the modalities. In this vein, many of the questions in the survey may have been ambiguous and elicited guesses from the participants, and thus the scores may fluctuate between positive and negative depending on their level of knowledge.
Finally, this study was conducted online and thus inadvertently targeted a technology-using portion of the population. Given the positive uptake of VR by those who are typically not considered ‘technology savvy’ (Riva, 2016 et al., Syed-Abdul et al., 2019), it is not thought that the perceptions found here would be significantly different to those if a paper-and-pencil survey was used.
This survey was disseminated to the young-adult university population who are at greater risk of developing an anxiety disorder and are thus more likely to consider engaging with VR and mobile app technologies for treatment. At large, a majority of responses indicate that individuals are optimistic about the role of technology in mental health and their use in treatment for anxiety, even without much supporting knowledge surrounding them. This suggests that VR and mobile apps are likely to be well received as they are validated with a sound evidence base and rolled out in various aspects of mental health. However, this survey highlights a potential higher level of uncertainty around the mediums for anxiety-experienced individuals. This result underscores the need to educate potential clientele on the technology’s scientific rigour, effectiveness and legitimacy to achieve best outcomes from therapy. As VR and mobile apps become increasingly well-known, future research should continue to assess the potentially shifting public perceptions, particularly within this age-range, and while accounting for experience with anxiety symptoms.
The authors would like to acknowledge the original academic staff who made the Global Leaders and Research Project (GLARP) possible to those from the Centre for Undergraduate Research Initiative for Excellence (CURIE) who contributed to our undergraduate research experience. A special thank you to Associate Professor Ernest Koh, Kate Aldred, Kirra Minton and Hannah Kirk for their help along the way. We would also like to acknowledge our additional original group member Lily Kennard for her contribution to GLARP. Finally, thank you to Dr Lucy Albertella for her support during the writing process.
Figure 1a: Awareness of VR in mental illness treatment
Figure 1b: Awareness of mobile apps in mental illness treatment
Figure 1c: Perception of VR as a legitimate treatment for mental illness
Figure 2: Perceived legitimacy of VR
Figure 3: Perceived effectiveness of VR
Figure 4a: Willingness to use VR if suggested by therapist
Figure 4b: Willingness to use VR
Figure 5: Perceived legitimacy of mobile apps
Figure 6: Perceived effectiveness of mobile apps
Figure 7a: Willingness to use mobile apps if suggested by therapist
Figure 7b: Willingness to use mobile apps as first point of help help-seeking contact
Figure 7c: Willingness to use mobile apps
Figure 8: Barriers to using VR and mobile apps
| How effective do you view VR as a treatment for anxiety? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 1.8 | 31.6 | 43.9 | 14.0 | 7.0 |
| Note: 1 = Not effective at all, 6 = Extremely effective | ||||||
| Do you view VR as an empirically legitimate method for psychological treatment? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 3.5 | 31.6 | 45.6 | 14.0 | 3.5 | 3.5 |
| Note: 1 = Not empirically legitimate at all, 6 = Extremely empirically legitimate | ||||||
| If VR were suggested by your therapist, how willing would you be to engage in treatment? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 3.5 | 5.3 | 21.1 | 35.1 | 35.1 |
| Note: 1 = Not willing to use at all, 6 = Extremely willing to use | ||||||
| How willing would you be to use VR as a sole method of treatment for anxiety symptoms? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 10.5 | 26.3 | 31.6 | 12.3 | 12.3 | 7.0 |
| Note: 1 = Not willing to use at all, 6 = Willing to use alone | ||||||
| How willing would you be to use VR as a method in conjunction with medication for treatment of anxiety symptoms? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 3.5 | 1.8 | 5.3 | 22.8 | 29.8 | 36.8 |
| Note: 1 = Not willing to use at all, 6 = Willing to use | ||||||
| Would you use VR as a method in conjunction with psychological therapy for treatment of anxiety symptoms? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 0.0 | 1.8 | 17.5 | 45.6 | 35.1 |
| Note: 1 = Not willing to use at all, 6 = Willing to use | ||||||
| How effective do you believe VR treatment alone is compared to medication for anxiety treatment? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 1.8 | 14.0 | 45.6 | 24.6 | 8.8 | 5.3 |
| Note: 1 = Not effective at all, 6 = More effective than medication | ||||||
| How effective do you believe VR is alone compared to psychological therapy such as Cognitive Behaviour Therapy (CBT)? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 19.3 | 40.4 | 28.1 | 8.8 | 3.5 |
| Note: 1 = Not effective at all, 6 = More effective than CBT | ||||||
Table 2: Perceptions on the effectiveness and legitimacy of mobile apps
| How effective do you view mobile apps as a treatment for anxiety? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 12.3 | 26.3 | 50.9 | 5.3 | 5.3 |
| Note: 1 = Not effective at all, 6 = Extremely effective | ||||||
| Do you view specifically designed mobile apps as an empirically legitimate method for psychological treatment? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 7.0 | 24.6 | 40.4 | 24.6 | 3.5 |
| Note: 1 = Not legitimate at all, 6 = Extremely legitimate | ||||||
| If a mobile app were suggested by your therapist, how willing would you be to engage in treatment? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 3.5 | 12.3 | 29.8 | 31.6 | 22.8 |
| Note: 1 = Not willing to use at all, 6 = Extremely willing to use | ||||||
| How willing would you be to use mobile apps as a sole method of treatment for anxiety symptoms? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 10.5 | 33.3 | 12.3 | 17.5 | 21.1 | 5.3 |
| Note: 1 = Not willing to use at all, 6 = Willing to use alone | ||||||
| As your first point of contact, how likely would you be to use mobile apps over contacting a medical practitioner or psychological therapist for help? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 7.0 | 19.3 | 19.3 | 19.3 | 15.8 | 19.3 |
| Note: 1 = Not willing to access first, 6 = Extremely willing to access first | ||||||
| How willing would you be to use mobile apps as a method in conjunction with medication for treatment of anxiety symptoms? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 8.8 | 8.8 | 29.8 | 28.1 | 24.6 |
| Note: 1 = Not willing to use at all, 6 = Willing to use | ||||||
| Would you use mobile apps as a method in conjunction with psychological therapy for treatment of anxiety symptoms? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 0.0 | 3.5 | 8.8 | 24.6 | 40.4 | 22.8 |
| Note: 1 = Not willing to use at all, 6 = Willing to use | ||||||
| How effective do you believe mobile apps are alone compared to medication for anxiety treatment? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 1.8 | 29.8 | 33.3 | 22.8 | 8.8 | 3.5 |
| Note: 1 = Not effective at all, 6 = More effective than medication | ||||||
| How effective do you believe mobile apps are alone compared to psychological therapy such as Cognitive Behaviour Therapy (CBT)? | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 42.1 | 15.8 | 12.3 | 14.0 | 14.0 | 1.8 |
| Note: 1 = Not effective at all, 6 = More effective than CBT | ||||||
Table 3: Barriers to use
| How concerned about the following would you be when using VR and / or mobile apps? | ||||||
| Motion sickness | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 42.1 | 15.8 | 12.3 | 14.0 | 14.0 | 1.8 |
| Vision complications | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 36.8 | 19.3 | 8.8 | 24.6 | 8.8 | 1.8 |
| Infections due to bacteria from sharing equipment | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 3.5 | 57.9 | 15.8 | 14.0 | 7.0 | 1.8 |
| Dizziness, vertigo | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 1.8 | 28.1 | 28.1 | 14.0 | 15.8 | 12.3 |
| Reliance on technology | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 33.3 | 22.8 | 22.8 | 12.3 | 7.0 | 1.8 |
| Confidentiality | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 35.1 | 26.3 | 19.3 | 8.8 | 10.5 | 0.0 |
| Note: 1 = Not concerned at all, 6 = Extremely concerned | ||||||
Table 4: Advantages to use
| How advantageous or better do you view VR for the following factors compared to current mainstream treatments (medications, psychological therapy)? | ||||||
| Accessibility for less-mobile individuals | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 12.3 | 5.3 | 24.6 | 19.3 | 19.3 | 19.3 |
| Accessibility for those with financial hardship | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 22.8 | 7.0 | 24.6 | 14.0 | 14.0 | 17.5 |
| Time commitment | ||||||
| Value | 1 | 2 | 3 | 4 | 5 | 6 |
| Per cent % | 12.3 | 14.0 | 26.3 | 14.0 | 17.5 | 15.8 |
| Note: 1 = No better than current treatments, 6 = Much better than current treatments. | ||||||
Alyami, M., B. Giri, H. Alyami and F. Sundram (2017). ‘Social anxiety apps: A systematic review and assessment of app descriptors across mobile store platforms’, Evidence-Based Mental Health, 20 (3), 65–70
Anderson, P., B. O. Rothbaum and L. F. Hodges (2003), ‘Virtual reality exposure in the treatment of social anxiety’, Cognitive and Behavioral Practice, 10 (3), 240–47
Arch, J. J., and M. G. Craske (2009), ‘First-line treatment: A critical appraisal of cognitive behavioral therapy developments and alternatives’, Psychiatric Clinics of North America, 32 (3), 525–47
Australian Bureau of Statistics (ABS) (2015), ‘4329. 0. 00. 004 National Health Survey: Mental Health and co-existing physical health conditions, Australia’, available at http://www.abs.gov.au/ausstats/abs@.nsf/0/C0A4290EF1E7E7FDCA257F1E001C0B84?Opendocument, accessed 11 July 2018
Australian Bureau of Statistics (ABS) (2018), ‘National Health Survey: First Results 2017–18’ available at https://www. abs. gov. au/ausstats/abs@. nsf/Lookup/by%20Subject/4364. 0. 55. 001~2017–18~Main%20Features~Mental%20and%20behavioural%20conditions~70, accessed 10 March 2020
Bouchard, S., J. St-Jacques, P. Renaud and B. K. Wiederhold (2009), ‘Side effects of immersions in virtual reality for people suffering from anxiety disorders’, Journal of CyberTherapy & Rehabilitation, 2 (2), 127
Bouchard, S., G. Robillard, I. Giroux, C. Jacques, C. Loranger, M. St-Pierre, M. Chrétien, and A. Goulet (2017). ‘Using virtual reality in the treatment of gambling disorder: The development of a new tool for cognitive behavior therapy’, Frontiers in Psychiatry, 8, 27
Botella, C., J. Fernández-Álvarez, V. Guillén, A. García-Palacios and R. Baños (2017). ‘Recent progress in virtual reality exposure therapy for phobias: A systematic review’, Current Psychiatry Reports, 19 (7), 42
Bystritsky, A. (2006), ‘Treatment‐resistant anxiety disorders’, Molecular Psychiatry, 11 (9), 805–14
Carl, E., A. T. Stein, A. Levihn-Coon, J. R. Pogue, B. Rothbaum, P. Emmelkamp and M. B. Powers (2019), ‘Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials’, Journal of Anxiety Disorders, 61, 27–36
Coates, D., C. Saleeba and D. Howe (2019), ‘Mental health attitudes and beliefs in a community sample on the central coast in Australia: Barriers to help seeking’, Community Mental Health Journal, 55 (3), 476–86
Coles, M. E., and S. L. Coleman (2010), ‘Barriers to treatment seeking for anxiety disorders: Initial data on the role of mental health literacy’, Depression and Anxiety, 27 (1), 63–71
Cote, S., and S. Bouchard (2008), ‘Virtual reality exposure for phobias: A critical review’, Journal of CyberTherapy and Rehabilitation, 1 (1), 75–92
Curcio, C., and D. Corboy (2020), ‘Stigma and anxiety disorders: A systematic review’, Stigma and Health, 5 (2), 125
David, D., I. Cristea and S. G. Hofmann (2018), ‘Why cognitive behavioral therapy is the current gold standard of psychotherapy’, Frontiers in Psychiatry, 9, 4
Donker, T., I. Cornelisz, C. Van Klaveren, A. Van Straten, P. Carlbring, P. Cuijpers, and J. L. Van Gelder (2019), ‘Effectiveness of self-guided app-based virtual reality cognitive behavior therapy for acrophobia: A randomized clinical trial’, JAMA Psychiatry, 76 (7), 682–90
Donker, T., K. Petrie, J. Proudfoot, J. Clarke, M. R. Birch and H. Christensen (2013), ‘Smartphones for smarter delivery of mental health programs: A systematic review’, Journal of Medical Internet Research, 15 (11), e247
Farach, F. J., L. D. Pruitt, J. J. Jun, A. B. Jerud, L. A. Zoellner and P. P. Roy-Byrne (2012), ‘Pharmacological treatment of anxiety disorders: Current treatments and future directions’, Journal of Anxiety Disorders, 26 (8), 833–43
Field, T. A., E. T. Beeson, L. K. Jones and R. Miller (2017), ‘Counselor allegiance and client expectancy in neuroscience-informed cognitive-behavior therapy: A 12–month qualitative follow-up’, Journal of Mental Health Counseling, 39 (4), 351–65
Firth, J., J. Torous, J. Nicholas, R. Carney, S. Rosenbaum, and J. Sarris, (2017), ‘Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials’, Journal of Affective Disorders, 218, 15–22
Garcia-Palacios, A., C. Botella, H. Hoffman and S. Fabregat (2007), ‘Comparing acceptance and refusal rates of virtual reality exposure vs. in vivo exposure by patients with specific phobias’ Cyberpsychology & Behavior, 10 (5), 722–24
Greenberg, R. P., M. J. Constantino and N. Bruce, N (2006), ‘Are patient expectations still relevant for psychotherapy process and outcome?’, Clinical Psychology Review, 26 (6), 657–78
Harris, M. G., M. J. Hobbs, P. M. Burgess, J. E. Pirkis, S. Diminic, D. J. Siskind, G. Andrews, and H. A. Whiteford (2015), ‘Frequency and quality of mental health treatment for affective and anxiety disorders among Australian adults’, Medical Journal of Australia, 202 (4), 185–89
Hofmann, S. G., A. Asnaani, I. J. J. Vonk, A. T. Sawyer and A. Fang (2012), ‘The efficacy of cognitive behavioral therapy: A review of meta-analyses’, Cognitive Therapy and Research, 36 (5), 427–40
Jorm, A. F. (2000), ‘Mental health literacy: Public knowledge and beliefs about mental disorders’, Br J Psychiatry, 177, 396–401
Kampmann, I. L., P. M. Emmelkamp, D. Hartanto, W. P. Brinkman, B. J. Zijlstra and N. Morina (2016), ‘Exposure to virtual social interactions in the treatment of social anxiety disorder: A randomized controlled trial’, Behaviour Research and Therapy, 77, 147–56
Keller, M. S., H. J. Park, M. E. Cunningham, J. E. Fouladian, M. Chen and B. M. R. Spiegel (2017), ‘Public perceptions regarding use of Virtual Reality in health care: A social media content analysis using Facebook’, Journal of Medical Internet Research, 19 (12), e419
Loerinc, A. G., A. E. Meuret, M. P. Twohig, D. Rosenfield, E. J. Bluett and M. G. Craske (2015), ‘Response rates for CBT for anxiety disorders: Need for standardized criteria’, Clinical Psychology Review, 42, 72–82
Lijster, J. M. D., B. Dierckx, E. M. Utens, F. C. Verhulst, C. Zieldorff, G. C. Dieleman and J. S. Legerstee (2017), ‘The age of onset of anxiety disorders: A meta-analysis’, The Canadian Journal of Psychiatry, 62 (4), 237–46
Lipschitz, J., C. J. Miller, T. P. Hogan, K. E. Burdick, R. Lippin-Foster, S. R. Simon and J. Burgess (2019), ‘Adoption of mobile apps for depression and anxiety: Cross-sectional survey study on patient interest and barriers to engagement’, JMIR Mental Health, 6 (1), 11334
Lui, J. H., D. K. Marcus and C. T. Barry (2017), ‘Evidence-based apps? A review of mental health mobile applications in a psychotherapy context’, Professional Psychology: Research and Practice, 48 (3), 199
McHugh, M. L. (2013), ‘The chi-square test of independence’, Biochemia Medica, 23 (2), 143–49
Morina, N., H. Ijntema, K. Meyerbröker and P. M. Emmelkamp (2015), ‘Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments’, Behaviour Research and Therapy, 74, 18–24
Nasir, B. F., M. R. Toombs, S. Kondalsamy-Chennakesavan, S. Kisely, N. S. Gill, E. Black, N. Hayman, G. Ranmuthugala, G. Beccaria, R. Ostini, and G. C. Nicholson (2018), ‘Common mental disorders among Indigenous people living in regional, remote and metropolitan Australia: A cross-sectional study’, BMJ Open, 8 (6), e020196
Osuch, E. A., E. Vingilis, C. Summerhurst, C. I. Forster, E. E. Ross, and A. J. Wrath (2015), ‘Process evaluation of an early-intervention program for mood and anxiety disorders among older adolescents and young adults’, Psychiatric Services, 66 (10), 1113–17
Overdijkink, S. B., A. V. Velu, A. N. Rosman, M. D. Van Beukering, M. Kok and R. P. Steegers-Theunissen (2018), ‘The usability and effectiveness of mobile health technology–based lifestyle and medical intervention apps supporting health care during pregnancy: systematic review’, JMIR mHealth and uHealth, 6 (4), e109
Parsons, T. D., and A. A. Rizzo (2008), ‘Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: A meta-analysis’, Journal of Behavior Therapy and Experimental Psychiatry, 39 (3), 250–61
Postolache, G., P. S. Girao, and O. Postolache (2014), ‘Applying smartphone apps to drive greater patient engagement in personalized physiotherapy’, in IEEE International Symposium on Medical Measurements and Applications (MeMeA), June 2014 Lisbon; IEEE, pp. 1–6
Postolache, O., F. Cary, P. S. Girão, and N. Duarte (2015), ‘Physiotherapy assessment based on Kinect and mobile APPs’, In 2015 6th International Conference on Information, Intelligence, Systems and Applications (IISA), July 2015, Corfu; IEEE, pp. 1–6
Reardon, T., K. Harvey, M. Baranowska, D. O’Brien, L. Smith, and C. Creswell (2017), ‘What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies’, European Child & Adolescent Psychiatry, 26 (6), 623–47
Riva, G., R. M. Baños, C. Botella, F. Mantovani, and A. Gaggioli (2016), ‘Transforming experience: the potential of augmented reality and virtual reality for enhancing personal and clinical change’, Front. Psychiatry, 7, 164
The Royal Australian and New Zealand College of Psychiatrists (RANZCP) (2014), ‘The economic cost of serious mental illness and comorbidities in Australia and New Zealand’, available at https://www.ranzcp.org/files/resources/reports/ranzcp-serious-mental-illness.aspx, accessed 10 March 2020
The Royal Australian and New Zealand College of Psychiatrists (RANZCP) (2015) ‘Minding the Gaps: Cost barriers to accessing health care for people with mental illness’, available at https://www.ranzcp.org/files/resources/reports/minding-the-gaps-cost-barriers-to-accessing-health.aspx, accessed 21 October 2020
Topper, M., P. M. Emmelkamp, E. Watkins, and T. Ehring, (2017), ‘Prevention of anxiety disorders and depression by targeting excessive worry and rumination in adolescents and young adults: A randomized controlled trial’, Behaviour Research and Therapy, 90, 123–36
Roy‐Byrne, P. (2015), ‘Treatment‐refractory anxiety; definition, risk factors, and treatment challenges’, Dialogues in Clinical Neuroscience, 17 (2), 191–206
Said, D., K. Kypri, and J. Bowman (2013). ‘Risk factors for mental disorder among university students in Australia: Findings from a web-based cross-sectional survey’, Social Psychiatry and Psychiatric Epidemiology, 48 (6), 935–44
Stolz, T., A. Schulz, T. Krieger, A. Vincent, A. Urech, C. Moser, S. Westermann, and T. Berger (2018), ‘A mobile app for social anxiety disorder: a three-arm randomized controlled trial comparing mobile and PC-based guided self-help interventions’, Journal of Consulting and Clinical Psychology, 86 (6), 493–504
Sucala, M., P. Cuijpers, F. Muench, R. Cardos, R. Soflau, A. Dobrean, P. Achimas-Cadariu, and D. David (2017), ‘Review of anxiety: There is an app for that. A systematic review of anxiety apps’, Depression and Anxiety, 34 (6), 518–25
Syed-Abdul, S., S. Malwade, A. A. Nursetyo, M. Sood, M. Bhatia, D. Barsasella, M. F. Liu, C.C. Chang, K. Srinivasan, M. Raja, and Y. C. J. Li, (2019). ‘Virtual reality among the elderly: A usefulness and acceptance study from Taiwan’, BMC Geriatrics, 19 (1), 223
Taylor, S., J. S. Abramowitz and D. McKay (2012), ‘Non-adherence and non-response in the treatment of anxiety disorders’, Journal of Anxiety Disorders, 26 (5), 583–89
Valmaggia, L. R., L. Latif, M. J. Kempton and M. Rus-Calafell (2016), ‘Virtual reality in the psychological treatment for mental health problems: A systematic review of recent evidence’, Psychiatry Research, 236, 189–95
Vogel, D. L., N. G. Wade and S. Haake (2006), ‘Measuring the self-stigma associated with seeking psychological help’, Journal of Counseling Psychology, 53, 325–37
Vogel, D. L., N. G. Wade and A. H. Hackler (2007), ‘Perceived public stigma and the willingness to seek counselling’, Journal of Counseling Psychology, 54, 40–50
Wampold, B. E., (2015), ‘How important are the common factors in psychotherapy? An update’, World Psychiatry, 14 (3), 270–77
Wang, K., D. S. Varma and M. Prosperi, (2018), ‘A systematic review of the effectiveness of mobile apps for monitoring and management of mental health symptoms or disorders’, Journal of Psychiatric Research, 107, 73–78
Weech, S., Kenny, S. and M. Barnett-Cowan (2019). ‘Presence and cybersickness in virtual reality are negatively related: A review’, Frontiers in Psychology, 10, 158
Zeng, N., Z. Pope, J. E. Lee, and Z. Gao (2018), ‘Virtual reality exercise for anxiety and depression: A preliminary review of current research in an emerging field’, Journal of Clinical Medicine, 7 (3), 42
Psychotherapy: The intentional engagement with a therapist for the purpose of healing, growth, transformation of a range of issues, including emotional and mental health concerns such as anxiety. It can take many forms and include talking, group work, art, movement and more. It aims to support and increase awareness in the client, facilitate development, growth, efficacy and enhance their wellbeing.
Pharmaceuticals: Any kind of drug used for medicinal or therapeutic purposes, such as to reduce the symptoms of anxiety.
Cognitive Behavioural Therapy (CBT): A type of psychotherapy which focuses on challenging and changing unhelpful ways of thinking, feeling and behaving. It aims to improve emotional regulation and help to develop personal coping strategies that target solving current problems.
Pharmacotherapy: The use of a drug for therapeutic purposes, such as to reduce the symptoms of anxiety.
Virtual reality (VR): A computer-generated simulation of a three-dimensional environment that can be interacted with in a seemingly real or physical way by a person. It is usually engaged with via electronic devices, such as special goggles with a screen or gloves fitted with sensors.
Stigma: A negative attitude or a mark of shame, disgrace or disapproval by other individuals, society or the self that results in an individual being or feeling rejected, discriminated against and excluded from participating in different areas of society.
To cite this paper please use the following details: Kirkham, R & Batten, C (2020), 'Public Perceptions on Using Virtual Reality and Mobile Apps in Anxiety Treatment: A cross sectional analysis', Reinvention: an International Journal of Undergraduate Research, Volume 13, Issue 2, https://reinventionjournal.org/article/view/625. Date accessed [insert date]. If you cite this article or use it in any teaching or other related activities please let us know by e-mailing us at Reinventionjournal@warwick.ac.uk.