
Bontu Yismawu Melaku, Zayed University; Fatme Al Anouti, Zayed University; Ala Al Rajabi,
Qatar University; Lynne Alexandra Kennedy, Zayed University
Adequate and timely folic acid intake can prevent the development of most Neural Tube Defects (NTDs) during pregnancy. However, up-to-date information on how much childbearing-age women are informed regarding this is limited in the United Arab Emirates. This study evaluated awareness and knowledge level of folate and folic acid (FA), along with FA supplement intake among female university students. It also assessed major demographic factors associated with knowledge of folate and with FA supplement usage, as well as examining participants’ risk level of inadequate folate intake. Of 239 female Zayed university students who completed the questionnaire, 63.2 per cent were aware of folate, and 44.8 per cent had good knowledge, but most (77 per cent) never took FA supplements consistently although the majority of the participants (38.5 per cent) were at higher risk of inadequate folate intake. Health science specialisation, history of folate deficiency or anaemia, and married or divorced marital status were associated with knowledge of folate/FA. Married/divorced marital status and history of folate deficiency or anaemia were also strongly correlated with FA supplement intake. However, pregnancy experience was not correlated with any of them. These results indicate a substantial gap in young women’s knowledge and FA supplementation. Therefore, effective education programmes are required to increase knowledge and promote folate-rich food consumption and FA intake.
Keywords: Dietary folate intake among undergraduates, awareness and knowledge of folate, folic acid supplementation among female students, demographic factors and knowledge of folate, demographic factors and folic acid supplementation, female university students and Vitamin B9
Neural tube defects (NTDs), like spina bifida and anencephaly, are among the common congenital disorders affecting the development of the spine and brain that result in early death or lifelong disability for a child (Cordero et al., 2015). However, the occurrence of most NTDs can be prevented if women consume adequate folic acid (FA) and dietary folate prior to and during pregnancy (Botto et al., 1999).
Folate is the generic term for vitamin B9 that encompasses both natural (dietary) folates found in foods and the synthetic form, FA, which is primarily used in food fortification and supplementation (Berry et al., 2010; Smith et al., 2008; Smith, 2023). Dietary folates occur naturally in a reduced, polyglutamate form. Before absorption, these are converted into monoglutamate forms in the intestine and transported to the liver, where they are reconverted to polyglutamates for storage or transformed into 5-methyltetrahydrofolate (5-methyl-THF) (McNulty, 2024). In contrast, FA exists in a fully oxidised, inactive monoglutamate form that can be easily absorbed in the intestine. However, since the biologically active folate involved in DNA synthesis and red blood cell production is reduced THF derivatives, typically present as polyglutamates (Smith et al., 2008), FA undergoes sequential reduction to dihydrofolate and then to tetrahydrofolate (THF). The produced THF is subsequently metabolised into intermediates that lead to the formation of 5-methyl-THF – the principal active form circulating in blood and supporting cellular metabolism (Scaglione and Panzavolta, 2014; Smith et al., 2008). Thus, folate deficiency and FA deficiency are used interchangeably to refer to insufficient availability of folate in the body.
Generally, FA has a substantially higher bioavailability than the natural (dietary) folates, being rapidly absorbed across the intestine (Smith et al., 2008), and is more stable to degradation on cooking, making it preferable for supplementation than the other folate forms.
Both dietary folate and FA, collectively referred to as folate, are used for red blood cell (RBC) and DNA synthesis in our bodies, and are essential for the development of neural tubes during the early stage of pregnancy (CDC, 2022; Smith et al., 2008). Inadequate folate intake can cause many health issues, including macrocytic anaemia and leukopenia, particularly due to impaired RBC formation, and risk of cardiovascular disease, cognitive dysfunction and liver disease associated with its DNA methylation/synthesis role (Yang et al., 2024). Also, folate status in the body is being linked to a broader range of clinical outcomes, including stroke, neurodevelopmental disorders, childhood leukaemia and lipid metabolism (Baddam et al., 2025). Besides this, folate deficiency in women is an important cause of NTDs in offspring, which are the second most common birth defects in humans (Wang et al., 2023). The incidence of NTDs is 0.5 to 5 per 1000 births (Wang et al., 2023), with 260,100 new NTDs cases in 2015 globally, of which 75 per cent (117,900) caused under-five mortality (Martinez et al., 2023), making the problem a critical issue that requires effective interventions.
Effective interventions such as mandatory food fortification and adequate FA supplement intake can help to significantly reduce the incidence of folate-deficiency-associated NTDs. Worldwide, 63 countries, including most countries in Latin America and Australasia, have adopted a mandatory policy for fortification of wheat flour, maize flour and/or rice with FA, although over 100 countries, including the majority of Europe, Asia and African countries had yet to implement the mandatory fortification policy in 2020 (Kancherla et al., 2022). The United Arab Emirates (UAE) also has not implemented a mandatory fortification policy with FA yet, although there is a voluntary fortification for wheat flour (Food Fortification Initiative, n.d.).
Effective and sufficient FA supplement intake can reduce the development of NTDs by 72 per cent and their recurrence in future pregnancies by 68 per cent (Bhutta et al., 2013). The World Health Organization (WHO) recommends that women take 400μg FA daily starting from before pregnancy until they are 12 weeks pregnant (World Health Organization, 2023). Various countries also have recommended 400μg daily FA intake from supplements for all childbearing-age women in addition to dietary folate intake (CDC, 2022; de Rosset et al., 2009; Kim et al., 2018). Regardless of this effort, a wide range of folate deficiency is still observed worldwide. Based on a systematic review of all nationally representative surveys that reported folate deficiency or insufficiency worldwide between 2000 and 2014, the prevalence of folate deficiency was 0–11 per cent in high-income countries, and 18–79 per cent in low-income countries (Martinez et al., 2023; Rogers et al., 2018). This can be partly associated with low FA supplementation among women. In many studies conducted across different countries, including Japan, Pakistan, Poland, Korea and Nigeria, a very low proportion of childbearing-age women (9–38 per cent) were found to take FA supplements during their periconceptional period (i.e. both prior to pregnancy and after conception), or before pregnancy (Chaudhri et al., 2019; Kim et al., 2018; Okon et al., 2020; Yamamoto and Wada, 2018; Zadarko-Domaradzka et al., 2021). FA supplement intake or supplementation refers to taking a FA supplement or a multivitamin containing FA regularly at the given time. Factors correlated with better FA supplementation include knowing FA’s benefit (Yamamoto and Wada, 2018) and its role in NTD prevention (Zadarko-Domaradzka et al., 2021), marriage and having pregnancy experience (Al-Mohaithef et al., 2021; Kim et al., 2018), older age (35 years old or more) (Yamamoto and Wada, 2018) and health science specialisation (Al-Mohaithef et al., 2021). However, the knowledge level of this population group regarding FA or folate was also reported as low, with only 8–43 per cent of women being identified as knowledgeable in many studies (Abdulrazzaq et al., 2003; Al-Mohaithef et al., 2021; Hisam et al. 2014; Kim et al., 2018; Zadarko-Domaradzka et al., 2021). Knowledge of FA and folate refers to knowing the benefits of FA during pregnancy, the recommended dose to take as a supplement, when the FA supplement should be taken in relation to the pregnancy period, and other related concepts. The low knowledge level and the insufficient FA supplement intake reported across the aforementioned studies underscore the necessity of giving priority to the issue and the need for further investigation of the topic to support effective health interventions.
Regarding the UAE, a recent finding from the United Arab Emirates Birth Cohort Study (UAEBCS) showed that folate intake of all first-trimester pregnant women of UAE nationals (100 per cent) was below the recommended dietary allowance (RDA) or adequate intake. Studies show an average intake of 112.9μg/day folate compared to the recommended amount of 600μg/day (Mutare et al., 2025), which indicates the importance of taking FA supplements to meet the need. However, up-to-date scientific literature on the FA supplementation of all childbearing-age women by including non-pregnant women and different nationalities is missing. Additionally, although awareness and knowledge of folic acid or folate have been significantly associated with an uptake in FA supplementation in women (Medawar et al., 2019; Sabi et al.,2022), evidence regarding the current awareness and knowledge level of childbearing-age women in the country – especially among those who have never had a pregnancy experience – is lacking. Awareness of FA or folate refers to having heard about FA or folate. To the best of the authors’ knowledge, only two studies (conducted in 2003 and 2010) of pregnant or postpartum women at healthcare centres are available, both reporting conflicting findings regarding prevalent awareness and knowledge level of FA (Abdulrazzaq et al., 2003; Al-Hossani et al., 2010). In the 2003 study, only 8.7 per cent of participants (i.e. postpartum women) knew about FA, particularly about its role, and only 46.4 per cent had heard about FA besides having insufficient FA supplementation (45.5 per cent) during their periconceptional period (preconception and in the first trimester) (Abdulrazzaq et al., 2003). A better result was reported later in the 2010 study, in which 66.7 per cent of pregnant women knew the importance of FA in pregnancy and 79.1 per cent had awareness of the nutrient, but only 7.8 per cent took FA supplement before their pregnancy (Al-Hossani et al., 2010). Regardless of these findings, the latest studies are missing in understanding the current awareness and knowledge of FA or folate, and the FA supplementation status of women in the country.
Additionally, the previous studies were conducted only at healthcare centres predominantly targeting pregnant or postpartum women, and did not consider the involvement of those who never had a pregnancy experience or have never married, which limits the generalisability of their findings to the general population of childbearing-age women.
As a result, this study aimed to fill existing evidence gaps by including childbearing-age women with diverse demographic characteristics, such as those who had never been pregnant or married, and by conducting the research in a university setting rather than a healthcare environment, thereby broadening the scope beyond previous studies that focused solely on pregnant or postpartum women. The study particularly focused on the childbearing-age university female students because of a high potential for early interventions, especially to reduce the risk of NTDs, in this population group.
The aim of the study was to evaluate the awareness and knowledge of dietary folate and FA, as well as the intake of FA supplements among female Zayed University students.
The objectives of the study were to:
This study was descriptive and correlational research conducted on 239 eligible Zayed University female students of both Abu Dhabi and Dubai campuses who were 16–40 years old. The data was collected online using Google Forms between 10 October and 2 November 2023. The required sample size was estimated as 359 using an online sample calculator tool, calculator.net, taking the population (all active childbearing-age women in both Zayed University campuses) size as 5264, confidence level as 95 per cent, margin of error as 5 per cent and population proportion as 50 per cent. The sample size calculator tool was used to ensure the study is fully powered by recruiting a sufficient number of participants to produce the true outcome and to ensure reproducibility of the outcomes (Althubaiti, 2022). To recruit the target participants, a list of 5264 actively enrolled female students on both campuses was obtained from the university’s registration office, and they were contacted through the institutional email system, inviting them to voluntarily participate in the study by completing the survey. The survey was administered online using Google Forms and designed to be self-administered. Volunteer participants were invited to complete the questionnaire anonymously and at their own convenience within the designated data-collection period. An invitation email, distributed through the university’s institutional email system, contained the survey link and detailed instructions for completion. An electronic participant information sheet was embedded within the survey, and informed consent was obtained electronically before participants were granted access to the questionnaire. This study was approved by the Research Ethics Committee at Zayed University, UAE (ZU23_062_S).
The survey consisted of a closed-ended multiple choice questionnaire adapted from previous successful studies (Alblowi and Alomayri, 2018; Kim et al., 2018), which had a similar aim and objectives as well as population characteristics as the current study, was used to collect data on awareness and knowledge of folate or FA, and FA supplement use, as well as related to the eating habits of the participants in addition to demographic characteristics.
The first part of the questionnaire included demographic characteristics (nationality, age, specialisation, income, marital status, pregnancy experience), personal history of folate or anaemia deficiency, and family history of congenital disorders. The second part assessed awareness and knowledge of folate and FA, the third part evaluated FA supplement use, while the fourth part examined the eating habits of the participants to determine their risk level of not taking adequate folate from food. The awareness domain question was ‘Have you heard about folic acid or folate?’, with yes/no options to choose from which were then assigned 0 and 1 values for analysis purpose (1 = yes, 0 = no); questions used to assess knowledge were, for example, ‘What is folic acid?’, with one correct and more incorrect options to choose from, which were then assigned 0 and 1 values for analysis (0 = for all incorrect options, 1 = correct option); the question used to evaluate FA supplement intake was ‘Do you take folic acid supplements or a vitamin containing folic acid regularly?’ and the options were yes/no which were then assigned 1 and 0 values (1 = yes, 0 = no) for analysis purpose. Additionally, the questions utilised to examine the risk level of inadequate folate intake were, for example, ‘In the past month, how often did you eat beans?’, along with five options (less than 3 times/month, 1–2 times/week, 3–4 times/week, 5–6 times/week, 1–2 times/day and 3 or more times/day), which were assigned a value 0 to 5 (0 = least frequent, 5 = most frequent). All these and the remaining utilised questions are included in the Appendix (at the end of this article).
FA or folate awareness was defined as having heard of FA or folate. Knowledge of FA and folate was defined as knowing that FA/folate prevents birth defects and that FA should be taken before pregnancy for the prevention of birth defects, that folate/FA is vitamin B, and other similar concepts. ‘Good knowledge’ was defined as answering half or more than half of the knowledge questions correctly, while ‘Poor knowledge’ was defined as answering less than half of the questions correctly. FA supplement intake (use) was defined as taking FA supplements or multivitamins containing FA regularly at the time of the study. Adequate folate intake (i.e. adequate dietary folate intake) was defined as reporting more frequent consumption of folate-rich foods; therefore, inadequate folate intake was defined as reporting lower-consumption frequencies on the eating habit checklist.
The data was analysed using SPSS version 29.0, and frequencies and percentages were calculated for categorical variables while percentiles were computed for numerical variables. Individuals who previously heard about folate or FA were considered to have awareness, and those who regularly took FA supplements or vitamins containing FA were assumed to have taken FA supplements (or have positive FA supplement usage or intake).
Knowledge was assessed by counting the total number of questions individuals answered correctly, and then by comparing everyone’s total number of questions answered correctly against half (50 per cent) of the knowledge questions. The total number of knowledge questions was six, so 50 per cent of the questions were three. Knowledge level was categorised into two: individual total counts of correctly answered questions equal to or more than 50 per cent of the knowledge questions (i.e. three) were grouped as ‘Good knowledge’, and those less than 50 per cent were classified as ‘Poor knowledge’.
While analysing the risk level of inadequate folate intake, scores were calculated at the individual level by adding up the values of selected options for all questions for each participant, and the obtained score was compared against the percentile scores of the sample population. The risk level was classified into three using the 33rd and 67th percentiles as cut-offs for the classification. Thus, individuals who scored less than or equal to 12 (i.e. 33rd percentile) were considered a high-risk group, those who scored from 13 to 16 (i.e., above the 33rd percentile up to the 67th percentile) by including both 13 and 16 considered as moderate risk, and those who scored greater than 16 were considered as a low-risk group. The significance of associations of demographic factors with awareness, knowledge, FA supplement intake and risk level of inadequate dietary folate intake was determined using chi-square test. However, where the assumption of the chi-square test was broken, fisher’s exact test (2-sided) and likelihood ratio were applied.
Out of the 5264 participants invited to participate, 239 participated in this study, matching a 67 per cent response rate. Demographic profiles of the participants (n = 239) were analysed and summarised with frequency and percentage as shown in Table 1. Most of them (97.1 per cent) were UAE nationals or Emiratis, 16–24 years old (95.8 per cent), and were studying fields outside of health science (63.6 per cent). Also, 93.3 per cent of the participants were single or never married. Most did not have a history of folate deficiency or anaemia (n = 149, 62.3 per cent), and only a few reported having a family member with a congenital disorder (13.4 per cent).

Table 1. Demographic characteristics of the participants (Authors’ collection)
Overall, 63.2 per cent of participants involved in this study were aware of folate or FA. However, the majority had poor knowledge (n = 132, 55.2 per cent), and those who had good knowledge about folate or FA were only 44.8 per cent, as shown in Figure 1. Among all of the participants, more than a third (41 per cent) knew that folate is a type of vitamin B, and 53.6 per cent knew that it helps with red blood production, neural tube formation, brain and spinal cord growth, and decreases miscarriage and preterm labour. Also, 52.3 per cent correctly identified the foods that are rich in folate. However, a higher proportion of the participants did not know the major health problems caused by FA deficiency during pregnancy (46.4 per cent), the appropriate period of taking FA for effective prevention of foetal malformations (53.6 per cent) and the daily recommended dose of FA for childbearing-age women (66.9 per cent).
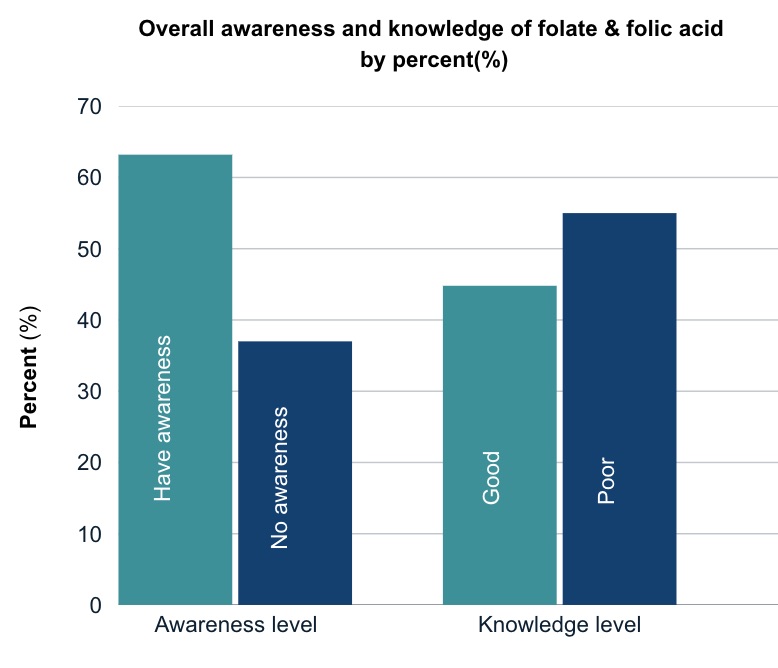
Figure 1. Overall awareness and knowledge level of folate and folic acid by per cent (%) (Authors’ collection)
As shown in Figure 2, common sources of information on folate and FA for participants were health professionals (38.9 per cent), family (31.4 per cent) and social media (22.2 per cent).
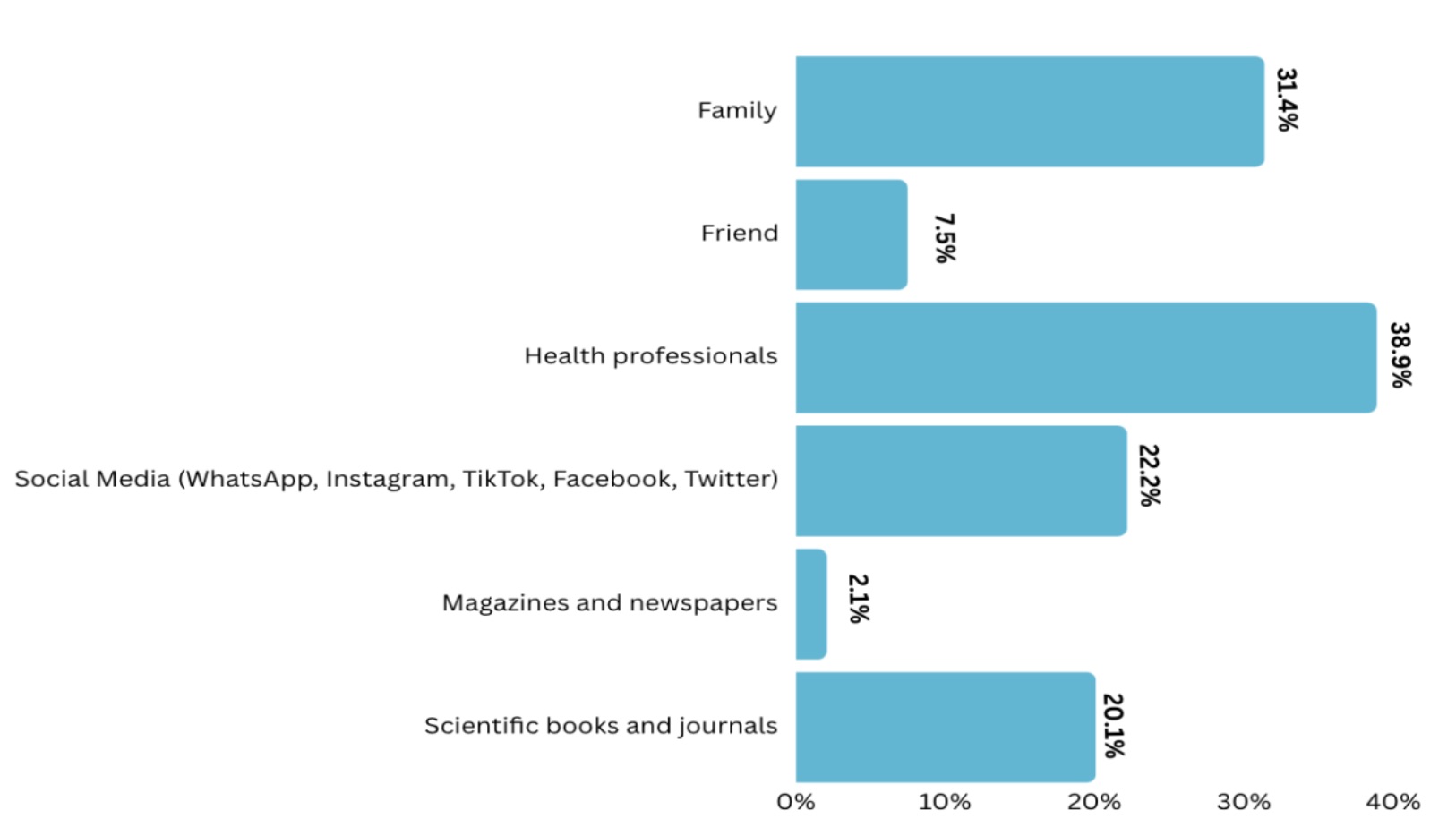
Figure 2. Common information sources of folate/FA (Authors’ collection)
More than three-quarters (77.0 per cent) of participants never regularly took FA supplements or vitamins containing FA (i.e. they had negative FA intake), as shown in Figure 3. Also, based on analysis of the eating habit checklist, the majority were at higher risk of inadequate folate intake (38.5 per cent), and those at moderate and lower risk were 29.3 per cent and 32.3 per cent respectively.
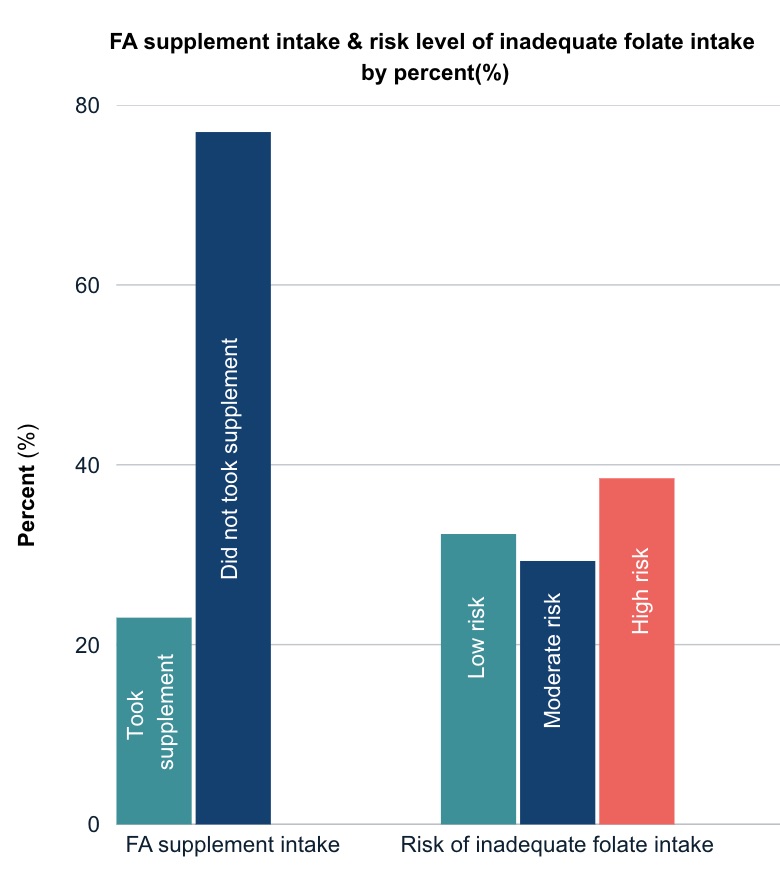
Figure 3. Level of folic acid (FA) supplementation and risk of inadequate folate intake among participants by per cent (%) (Authors’ collection)
A significantly higher proportion of individuals enrolled in health science field, and those with a history of folate deficiency or anaemia, had heard about folate or FA (i.e. had awareness) compared to those enrolled in non-health-related fields and those with no history of folate deficiency or anaemia (p < 0.001 and p = 0.048, respectively) (see Table 2). Those participants were also identified as being more knowledgeable (p < 0.001, and p = 0.026 respectively) along with married or divorced women (p = 0.046), as shown in Table 2. However, no significant difference in knowledge was observed in terms of nationality (p = 1.000), age (p = 0.518), pregnancy experience (p = 0.282) or having family members with congenital abnormalities or not (p = 0.374).
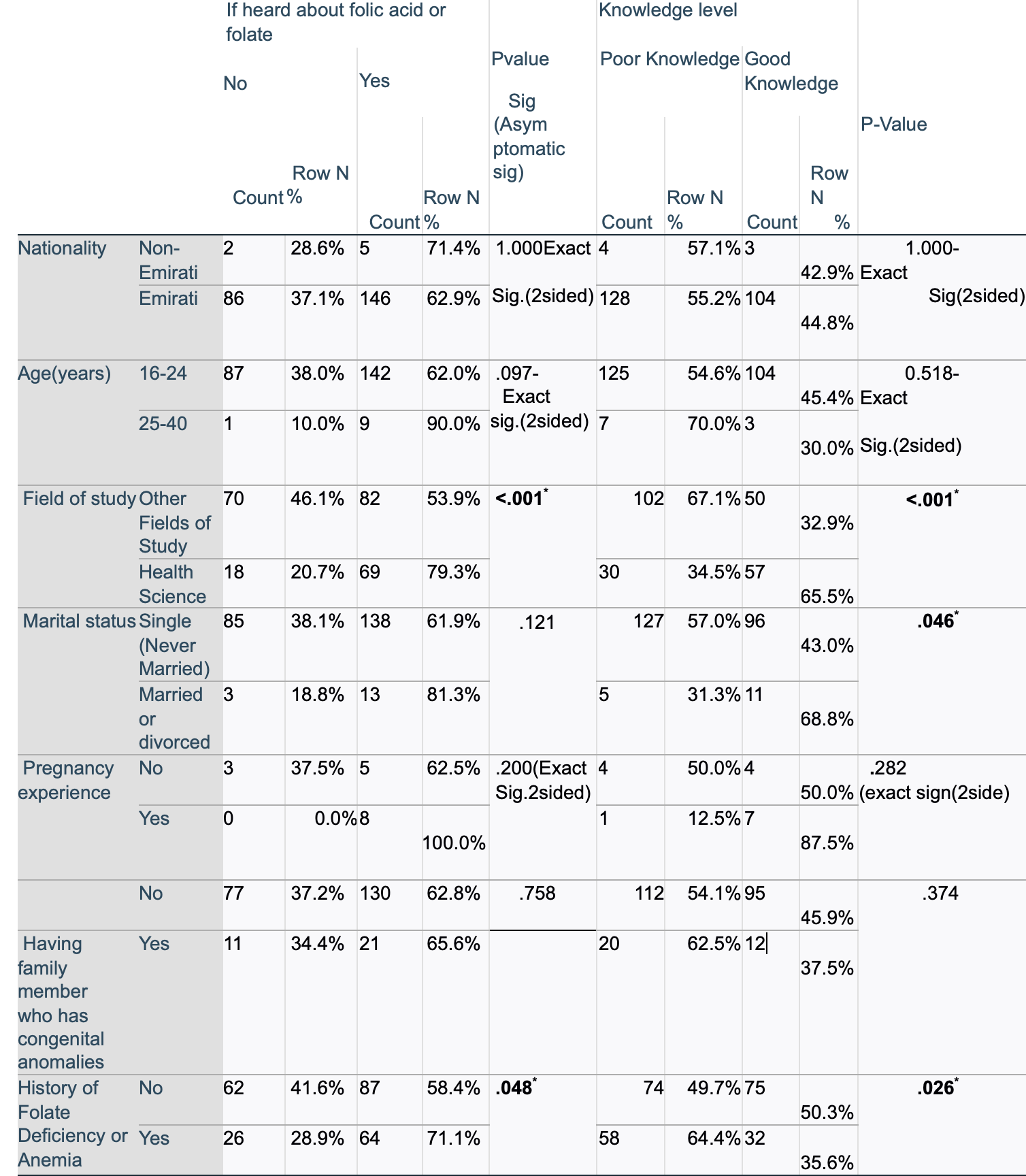
Table 2.The association of demographic factors with awareness and knowledge of folate or folic acid (Authors’ collection)
Note: Star (*) shows the p-value is ≤ 0.05 and it is statistically significant.
Taking FA supplements or vitamins containing FA was statistically highly associated with being married or divorced (p < 0.001) and having a history of folate deficiency or anaemia (p = 0.003), as shown in Table 3. In contrast, no significant difference in terms of FA supplementation was observed among individuals with different nationalities (p = 0.729), age groups (p = 0.244), fields of study (p = 0.335), pregnancy experiences (p = 0.119), and having a family member with a congenital disorder or not (p = 0.460). Similarly, none of the factors, except having pregnancy experience (p = 0.010), were significantly associated with the risk level of inadequate folate intake.
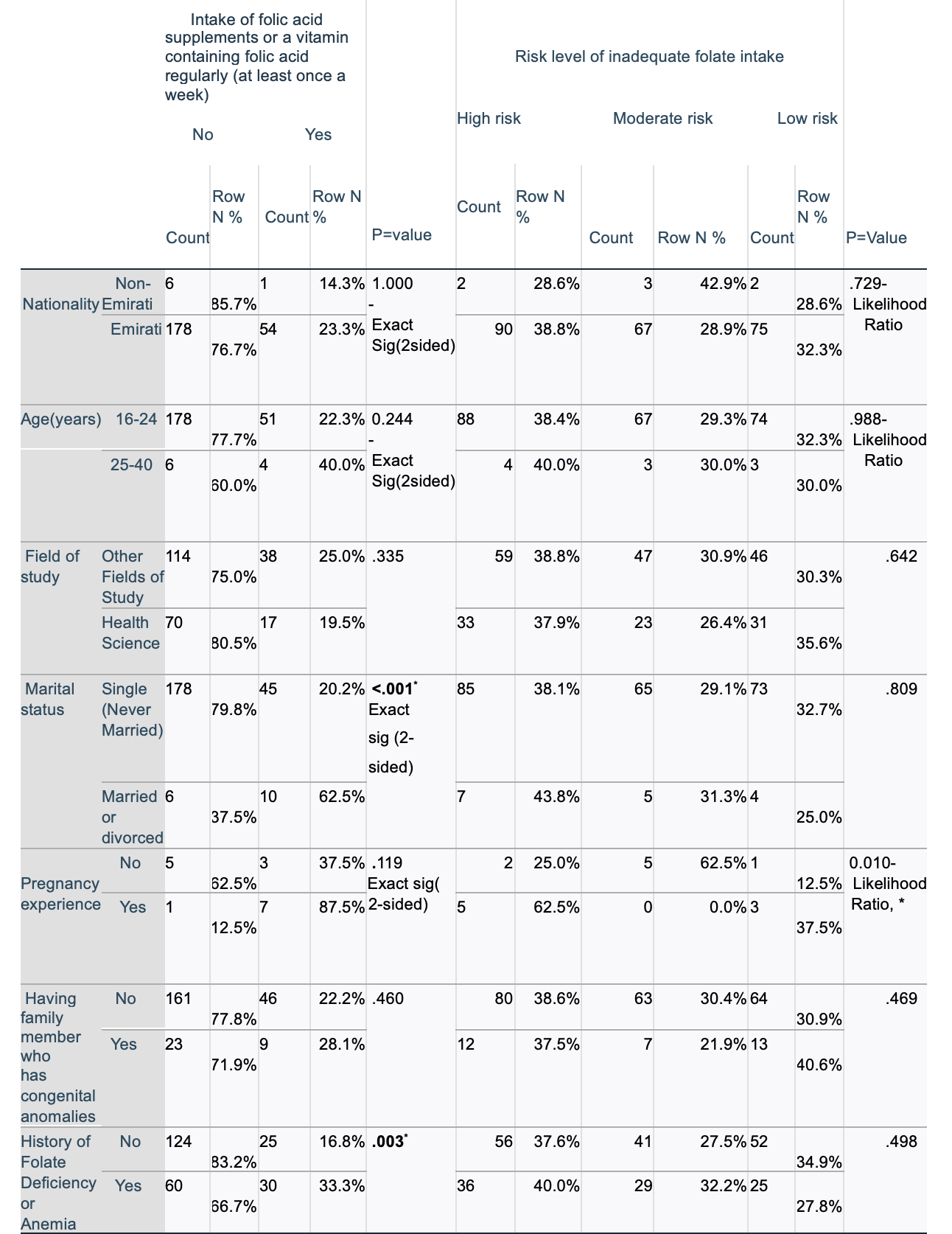 Table 3. Association of demographic factors with folic acid intake level and risk level of inadequate folate intake (Authors’ collection)
Table 3. Association of demographic factors with folic acid intake level and risk level of inadequate folate intake (Authors’ collection)
Note: Star (*) shows the p-value is ≤ 0.05 and it is statistically significant.
This study found a good awareness level of folate/FA (63.2 per cent) among participants. However, this result was lower than the finding of a previous study conducted in the UAE in 2010 where 79 per cent of participants had heard about FA (Al-Hossani et al., 2010). This difference may be attributed to the population of the study. The previous study was conducted among pregnant or married women (Al-Hossani et al., 2010), groups who are more likely to receive formal information from healthcare providers during clinic visits. In contrast, the current study primarily involved single or never-married university students who have fewer opportunities to access such information through healthcare settings.
In the current study, less than half (44.8 per cent) of the participants had good knowledge of folate and FA regardless of their higher education level, which is approximately comparable to the 38.3 per cent knowledge level reported by Al-Mohaithef et al. (2021) from the Saudi Electronic University in Saudi Arabia. Regarding knowledge of specific aspects of folate and FA, 41 per cent of the current study’s participants knew that folate is vitamin B, 53.6 per cent of them correctly identified the benefits of FA, and more than half (52.3 per cent) could distinguish foods rich in folate. This agrees with previous study findings of Alblowi and Alomayri (2018) where 31.7 per cent of participants knew the food group of folate, and 54.5 per cent could state that vitamin B helps with neural tube formation and brain and spinal cord growth. However, in the current study, the majority of the participants did not know the recommended dose of FA from the supplement (66.9 per cent), when FA supplement should be taken for effective prevention of malformations during pregnancy (53.6 per cent), and the major health problems FA deficiency can cause in a foetus (46.4 per cent). This finding is supported by evidence from a 2013 study conducted in the UAE, which reported that only 42 per cent of Emirati women were aware of the importance and benefits of FA intake prior to conception, and 51 per cent were unaware of the appropriate timing for supplementation (Alkaabi et al., 2013; Mutare et al., 2025). This underscores the necessity of education and awareness programmes to increase awareness and knowledge of folate or FA among young adult women across the UAE.
The current study found that only 23 per cent of the participants took FA supplements. This is slightly higher than the previous finding reported in 2010 within the UAE, where only 7.8 per cent of participants reported taking FA supplements prior to pregnancy (Al-Hossani et al., 2010). However, the current finding is lower by more than half compared to a recent finding in the region among university students (47.1 per cent), particularly at Saudi Electronic University in Saudi Arabia (Al-Mohaithef et al., 2021). This observed difference could be due to differences in demographic profiles of the study population between the two studies, besides differences in the study setting. In Al-Mohaithef et al.’s study, the majority of the participants were married (53.8 per cent), and many of them were pregnant or had a history of pregnancy (49 per cent), unlike in the current study in which most were single or never married (93.3 per cent), and only 3.35 per cent had a history of pregnancy.
Studies have shown that awareness or knowledge of FA is significantly associated with women’s FA supplement intake (Chaudhri et al., 2019; Hisam et al., 2014; Kim et al., 2018; Sabi et al., 2022). Therefore, to promote adequate FA supplement uptake in the UAE, effective education campaigns on the benefits of FA by targeting all childbearing-age women – especially those who are unmarried and therefore less likely to receive information during clinical visits – are needed.
The current study also found that a higher percentage of the participants (38.5 per cent) were at higher risk of inadequate folate intake, with those at moderate risk being 29.3 per cent while those at low risk were only 32.3 per cent. This was opposite to the findings of Kim et al. (2018), where the majority of the participants (37.4 per cent) were at low risk of inadequate folate intake from food, and those at higher risk were 31.8 per cent. The heightened risk of inadequate folate intake observed in the current study may be partly linked to the widespread adoption of Western dietary patterns, consisting of fast foods and sweets with low folate content, in the UAE. The country has undergone a rapid shift from traditional food habits and active lifestyles to Westernised diets and more sedentary behaviours (Mutare et al., 2025). A recent study among first-trimester pregnant Emirati women highlighted these changes, reporting that over half (56 per cent) exceeded the acceptable macronutrient distribution range (AMDR) for saturated fat, while the vast majority (94 per cent) consumed only about 10g of dietary fibre per day – far below the recommended 28g/day (Mutare et al., 2025). Therefore, given the poor knowledge level found in the current study that might have contributed to the higher risk level, health professionals, who were identified as a major source of information (38.9 per cent), should strive to deliver accurate and in-depth information regarding folate and FA to the young adult women and their families. Also, families, as the second most common source of information reported in this survey (31.4 per cent), should be willing to learn about FA and folate as well as health in general, and share the information with their children responsibly.
Based on the chi-square test, this study found that health science students and individuals who have a history of folate deficiency or anaemia were significantly more aware and knowledgeable of folate or FA than those whose field of study was different from health science and those who did not have a history of folate deficiency or anaemia. Similarly, married or divorced women had higher knowledge levels compared to those who never married. However, age, nationality and pregnancy experiences were not associated with both knowledge and awareness of folate or FA, although some previous studies reported the presence of an association; for instance, Abdulrazzaq et al. (2003) reported greater knowledge among non-UAE nationals compared to other nationalities. However, this disagreement could be due to a small proportion of different nationalities represented in the current study.
Regarding factors associated with FA supplement usage, Fisher’s exact test indicated that married or divorced individuals were significant FA supplement users, while the chi-square test showed that those with a history of folate deficiency or anaemia also had positive FA supplement intake. However, the current study did not find a significant association between FA supplementation and older age, health science specialisation, as well as pregnancy experience, although previous studies reported them to be associated with greater FA supplement usage (Al-Mohaithef et al., 2021; Kim et al.,2018; Yamamoto and Wada, 2018). This observed difference might be due to the small representation of individuals with older age and pregnancy experience in this study, so further studies with better representation are required. This research also found that individuals who had pregnancy experience were at higher risk of inadequate folate intake, which highlights the need for targeted education to enhance their knowledge level and, in turn, their FA intake before their next pregnancy.
The average monthly income of the household and having a child with congenital anomalies were not tested for association with awareness, knowledge and use of FA supplements or folate intake from food. The reason is that most of the participants responded that they do not know or prefer not to tell the average monthly income, and none of them has ever had a child with a congenital disorder.
In general, this study has effectively answered the main research question by identifying the level of awareness and knowledge of folate/FA and FA supplement usage among female Zayed University students. It also successfully evaluated the risk level of inadequate folate intake and distinguished the major demographic factors associated with knowledge level and FA supplementation among participants. To the best of the authors’ knowledge, this is the first study investigating awareness, knowledge of folate/FA, and FA supplements among female university students in the UAE.
The limitation of this study is that the number of married or divorced women, those who had experience of pregnancy, and non-UAE nationals was small or underrepresented; thus, interpretation of the conclusions regarding the association of these factors with knowledge of FA/folate and intake of FA supplements requires caution. Also, students were not asked in which year of their academic programme they were, which might have an impact on the generalisability of the result to the target population. Finally, a pilot study was not carried out in this study to test the validity of the questionnaire, especially for the questions used to assess the risk level of inadequate folate intake. Also, to assess the knowledge, one item asked ‘Which health problem can mainly occur due to FA deficiency during pregnancy?’ with options including neural tube defects/spinal cord defects, anaemia and low birth weight. However, because more than one option is defensible, the wording (‘mainly’) and single-best-answer format might have introduced content ambiguity and misclassification of individuals who chose a scientifically defensible, but non-expected, response. As a result, participants who selected a valid but non-expected answer could have received a lower score on this item, and in turn overall knowledge score below the cut-off. Consequently, these individuals may have been incorrectly classified as having ‘poor knowledge’ although their responses reflected a reasonable understanding of folic acid deficiency. This may have attenuated observed associations between knowledge and covariates. To evaluate its impact, the authors reclassified knowledge after excluding this item while retaining the cut-off (a priori rule of) ≥50 per cent considered as ‘Good knowledge’ level. The numerical cut-off shifted from 3/6 to 2.5/5; however, because individual scores are integers, the operational threshold remained ≥3 correct. Consequently, the proportions categorised as good vs poor knowledge were unchanged; thus, the knowledge outcomes without excluding the item were kept. However, the authors acknowledge this measurement limitation and the need for caution when interpreting the knowledge result. Additionally, the use of tertiles (i.e. 33rd and 67th percentiles) as cut-off to classify the risk level of inadequate dietary folate intake in this study, mainly yields relative, sample-dependent ranking rather than an absolute indicator of inadequacy. Therefore, the obtained estimates may be less comparable across studies and may misclassify individuals near clinically meaningful thresholds.
The authors express sincere gratitude to Dr Rafiq Hizaji for his invaluable support in the data analysis and all participants for taking part in this study.
Figure 1. Overall awareness and knowledge level of folate and folic acid by per cent (%)
Figure 2. Common information sources of folate/FA.
Figure 3. Level of folic acid (FA) supplementation and risk of inadequate folate intake among participants by per cent (%)
(All figures are produced by the authors)
Table 1. Demographic characteristics of the participants
Table 2. The association of demographic factors with Awareness and knowledge of folate or folic acid
Table 3. Association of demographic factors with folic acid intake level, and risk level of inadequate folate intake
Awareness and knowledge about folic acid
1. Have you heard about folic acid or folate? (Awareness)
2. What is folic acid? – Knowledge (K)
3. What is the benefit of folic acid? – K
4. Which health problem can mainly occur by folic acid deficiency during pregnancy? – K
5. When should folic acid be taken for effective prevention of foetus malformations? – K
6. Which of the following foods is (are) a rich source of folate – K
7. What is the dose of folic acid required daily for a woman planning to conceive or for a pregnant woman? – K
8. From whom did you hear about the importance of folic acid? (Please tick all that apply)
Intake of Folic Acid supplements
1. Do you take folic acid supplements or a vitamin containing folic acid regularly (at least once a week)?
Risk level of inadequate folate intake
1. In the past month, how often did you eat 3 meals per day? (Most frequent is desirable)
2. In the past month, how often did you have enough time for breakfast?
3. In the past month, how often did you eat rice?
4. In the past month, how often did you eat or drink oranges/orange juices?
5. In the past month, how often did you drink milk?
6. In the past month, how often did you eat meat (such as liver, chicken giblets, etc.)?
7. In the past month, how often did you eat beans?
8. In the past month, how often did you eat green vegetables (e.g. spinach, broccoli, asparagus, cabbage, etc.)?
Abdulrazzaq, Y. M., L. I. Al-Gazali, A. Bener, M. Hossein, M. Verghese, A. Dawodu and Padmanabhan, R. (2003), ‘Folic acid awareness and intake survey in the United Arab Emirates’, Reproductive Toxicology (Elmsford, N.Y.), 17 (2), 171–76.
Alblowi, S. A. and M. H. Alomayri (2018), ‘Assessment of knowledge, awareness and behavior of folic acid use among females during the childbearing period in Tabuk City – 2017’, The Egyptian Journal of Hospital Medicine, 70 (7), 1242–47.
Al-Hossani, H., H. Abouzeid, M. M. Salah, H. M. Farag and E. Fawzy (2010), ‘Knowledge and practices of pregnant women about folic acid in pregnancy in Abu Dhabi, United Arab Emirates’, Eastern Mediterranean Health Journal = La revue de sante de Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit,16 (4),402–07.
Alkaabi, M. S., L. K. Alsenaidi and H. Mirghani (2013), ‘Awareness and knowledge of the use and benefits of folic acid supplements in women in the United Arab Emirates’, Hamdan Medical Journal, 6 (3), 385–88.
Al-Mohaithef, M., H. Alaslani, N. B. Javed and S. Chandramohan (2021), ‘Folic acid awareness and usage among females at Saudi Electronic University in Jeddah, Saudi Arabia’, SAGEopenmedicine, 9, 20503121211059682.
Althubaiti, A. (2022), 'Sample size determination: A practical guide for health researchers', Journal of General and Family Medicine, 24 (2), 72–78. https://doi.org/10.1002/jgf2.600
Baddam, S., K. M. Khan and I. Jialal (2025), ‘Folic acid deficiency’, StatPearls [internet], Treasure Island, FL: StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK535377/
Berry, R. J., L. Bailey, J. Mulinare, C. Bower and O. Dary (2010), ‘Fortification of flour with folic acid’, Food Nutr Bull. (1 Suppl), S22–35. https://doi.org/10.1177/15648265100311S103.
Bhutta, Z. A., J. K. Das, A. Rizvi, M. F. Gaffey, N. Walker, S. Horton, P. Webb, A. Lartey, R. E. Black and Lancet Nutrition Interventions Review Group, the Maternal and Child Nutrition Study Group (2013), ‘Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost?’, Lancet (London, England), 382 (9890), 452–77.
Botto, L. D., C. A. Moore, M. J. Khoury and J. D. Erickson (1999), ‘Neural-tube defects’, The New England Journal of Medicine, 341 (20), 1509–19.
Cambridge Dictionary (n.d.), available at https://dictionary.cambridge.org/dictionary/english, accessed on 29 October 2025.
(CDC) Center for Disease Control, (2022), ‘Folic acid: Why folic acid is important before and during pregnancy’, available at https://www.cdc.gov/ncbddd/folicacid/about.html#:~:text=When%20the%20baby%20is%20developing,t he%20early%20brain%20and%20spine, accessed on 1 May 2023.
Chaudhri, D. S., D. J. Kamran, D. R. Atif, D. R. Gillani, D. S. Ihsan, D. A. Shahid and D. H. Inam (2019), ‘Knowledge and usage pattern of folic acid among medical students of Rawalpindi’, Pakistan Armed Forces Medical Journal, 69 (SUPPL2), S297–302.
Cordero, A. M., K. S. Crider, L. M. Rogers, M. J. Cannon and R. J. Berry (2015), ‘Optimal serum and red blood cell folate concentrations in women of reproductive age for prevention of neural tube defects: World Health Organization guidelines’, MMWR Morbidity and Mortality Weekly Report, 64 (15), 421–23.
de Rosset, L., A. Mullenix and L. Zhang (2009), ‘Multivitamins, folic acid and birth defects: Knowledge, beliefs and behaviors of Hispanic women in North Carolina’, American Journal of Health Education, 40 (3), 155–64.
Food Fortification Initiative (n.d.), ‘Country profile: United Arab Emirates’, available at https://www.ffinetwork.org/united-arab-emirates/?record=225, accessed on 15 October 2025
Hisam, A., M. U. Rahman and S. F. Mashhadi (2014), ‘Knowledge, attitude and practice regarding folic acid deficiency; A hidden hunger’, Pakistan Journal of Medical Sciences, 30 (3), 583–88.
Kancherla, V., K. Wagh, P. Priyadarshini, H. Pachón and G. P. Oakley Jr. (2022), ‘A global update on the status of prevention of folic acid-preventable spina bifida and anencephaly in year 2020: 30-Year anniversary of gaining knowledge about folic acid’s prevention potential for neural tube defects’, Birth Defects Research, 114 (20), 1392–403, https://doi.org/10.1002/bdr2.2115
Kim, M. J., J. Kim, E. J. Hwang, Y. Song, H. Kim and T. Hyun (2018), ‘Awareness, knowledge, and use of folic acid among non-pregnant Korean women of childbearing age’, Nutrition Research and Practice, 12 (1), 78–84.
Martinez, H., A. Benavides-Lara, A. Arynchyna-Smith, K. A. Ghotme, M. Arabi and A. Arynchyn (2023), ‘Global strategies for the prevention of neural tube defects through the improvement of folate status in women of reproductive age’, Child’s Nervous System, 39 (7), 1719–36. https://doi.org/10.1007/s00381-023-05913-4
McNulty, H. (2024), ‘Folate’, in R. S. Gibson (ed.), Principles of Nutritional Assessment (3rd ed.), available at https://nutritionalassessment.org/folate/, accessed on 15 October 2025
Medawar, G., T. Wehbe and E. A. Jaoude (2019), ‘Awareness and use of folic acid among women of childbearing age’, Annals of Global Health, 85 (1), 54.
MedlinePlus Medical Encyclopedia (2023), ‘Folic acid in diet’, available at https://medlineplus.gov/ency/article/002408.htm, accessed on 27 June 2024
Mutare, S., M. Mohamad, J. Feehan, L. Cheikh Ismail, H. I. Ali, L. Stojanovska, H. Khair, A. Shehab, R. Ali, N. Hwalla, S. Kharroubi, A. Hills, M. Fernandes, S. Al Neyadi and A. S. Al Dhaheri (2025), ‘First-trimester nutrition insights from the United Arab Emirate Birth Cohort Study (UAE-BCS): Assessment of dietary intake, micronutrient profiles, and folic acid supplementation in Emirati Women’, Journal of Nutritional Science, 14, e24. https://doi.org/10.1017/jns.2025.11
Okon, U. A., B. S. Ibrahim, R. Usman, E. Adedire, M. S. Balogun and A. Olayinka (2020), ‘Awareness and use of folic acid among women of childbearing age in Benue State, Nigeria’, The Pan African Medical Journal, 37, 60.
Rogers, L. M., A. M. Cordero, C. M. Pfeiffer, D. B. Hausman, B. L. Tsang, L. M. De-Regil, J. Rosenthal, H. Razzaghi, E. C. Wong, A. P. Weakland and L. B. Bailey (2018), ‘Global folate status in women of reproductive age: A systematic review with emphasis on methodological issues’, Annals of the New York Academy of Sciences, 1431 (1), 35–57.
Sabi, E. M., A. H. Mujamammi, N. Alturki, T. Alzaid, A. Almutairi, R. Algarni, D. Almaziad, N. Alhumaidhi, Z. Kurdee and K. M. Sumaily (2022), ‘Level of knowledge and awareness of female undergraduate students and determinants of knowledge of folic acid and supplementation’, Medicina, 58 (8), 986.
Scaglione, F. and G. Panzavolta (2014), ‘Folate, folic acid and 5-methyltetrahydrofolate are not the same thing’, Xenobiotica, 44 (5), 480–88. https://doi.org/10.3109/00498254.2013.845705
Smith, A. D., Y.-I. Kim and H. Refsum (2008), ‘Is folic acid good for everyone?’ The American Journal of Clinical Nutrition, 87 (3), 517–33. https://doi.org/10.1093/ajcn/87.3.517
Smith, D. J. M. (2023), ‘Folate and folic acid metabolism: a significant nutrient-gene-environment interaction’, Medical Research Archives, 11 (5), https://doi.org/10.18103/mra.v11i5.3824
Wang, X., J. Yu and J. Wang (2023), ‘Neural tube defects and folate deficiency: Is DNA repair defective?’ International Journal of Molecular Sciences, 24 (3), 2220, https://doi.org/10.3390/ijms24032220
World Health Organization. (2023), ‘Periconceptional folic acid supplementation to prevent neural tube defects’, e_Library of Evidence for Nutrition Actions (eLENA), available at https://www.who.int/tools/elena/interventions/folate-periconceptional, accessed 16 October 2023
Yamamoto, S. and Y. Wada (2018), ‘Awareness, use and information sources of folic acid supplementation to prevent neural tube defects in pregnant Japanese women’, Public Health Nutrition, 21 (4), 732–39.
Yang, M., D. Wang, X. Wang, J. Mei and Q. Gong (2024), ‘Role of folate in liver diseases’, Nutrients, 16 (12), 1872, https://doi.org/10.3390/nu16121872
Zadarko-Domaradzka, M., E. Kruszyńska and E. Zadarko (2021), ‘Effectiveness of folic acid supplementation recommendations among Polish female students from the Podkarpackie region’, Nutrients, 13 (3), 1001.
Awareness and knowledge of folic acid or folate: Having heard the term ‘folate’ or ‘folic acid’ (FA) at any time.
Congenital disorder: Defects or abnormalities in the baby’s body that develop during pregnancy.
Content ambiguity: A situation in which a statement can be understood in more than one way and may therefore cause confusion.
Folate: Generic term for vitamin B9 that encompasses both natural (dietary) folates found in foods and the synthetic form, folic acid (FA), which is primarily used in food fortification and supplementation. Dietary folate is naturally found in foods such as green leafy vegetables, beans, liver and fresh fruits (MedlinePlus, 2023).
Folic acid: A synthetic form of folate usually taken as a supplement or by consuming fortified foods. Also known as FA.
Neural tube: A structure that is formed in the foetus during the early stage of pregnancy, usually before the 6th week of conception, and later develops into the baby’s spinal cord, spine, brain, and skull. At early stage of the pregnancy, normally, these tubes are closed, but failure of their closure causes a disability called neural tube defects.
Neural tube defects: Defects on the brain and spinal cord of a baby that develop due to improper closure of the neural tubes during the first month of pregnancy and the problem is mainly linked to folate deficiency in the baby’s mother. Also known as NTDs.
Misclassification: Refers to the incorrect categorization of individuals. In this study’s context, it refers to assigning participants to the ‘poor knowledge’ of folate category when, in the absence of questionnaire design limitations, they would more accurately have been classified as having ‘good knowledge.’
Monoglutamate: A Folate molecule containing only one glutamic acid residue in its structure (McNulty, 2024)
Polyglutamate: A folate molecule containing multiple glutamate residues or units in its structure (McNulty, 2024).
To cite this paper please use the following details: Melaku, B.Y., Anouti, F.A., Rajabi, A.A., Kennedy, L.A. (2025), 'Awareness, Knowledge and Practice of Female Zayed University Students Regarding Folate and Folic Acid', Reinvention: an International Journal of Undergraduate Research, Volume 18, Issue 2, https://reinventionjournal.org/index.php/reinvention/article/view/1719. Date accessed [insert date]. If you cite this article or use it in any teaching or other related activities, please let us know by emailing us at Reinventionjournal@warwick.ac.uk.
https://doi.org/10.31273/reinvention.v18i2.1719, ISSN 1755-7429, © 2025, contact reinventionjournal@warwick.ac.uk. Published by the Institute for Advanced Teaching and Learning, University of Warwick. This is an open access article under the CC-BY licence (https://creativecommons.org/licenses/by/4.0/)