Halima Nabirye, Muni University
Breast self-examination (BSE) is an effective, inexpensive and simple screening technique for examining breasts monthly to detect breast cancer. Among women diagnosed with breast cancer in Uganda, 89 per cent of them present with stage III or IV, which has a poor prognosis. This study was conducted to assess knowledge, attitudes and barriers regarding BSE among women in Nyio ward, Arua City, Uganda.
A descriptive cross-sectional study was conducted among 354 women selected by cluster sampling and random walk method. Data was entered into Microsoft Excel, coded and analysed using the SPSS version 23. Knowledge of BSE among the participants was low. Less than half of the respondents (47.5 per cent) had ever heard about BSE as means of early detection of breast cancer and only 23.2 per cent knew how to perform BSE. The majority (95.8 per cent) had a positive attitude towards BSE practice, 85.7 per cent believed BSE is crucial in detecting breast cancer early, and most (83.3 per cent) agreed early detection increases the chances of long-term survival. The most common barrier towards BSE was lack of awareness.
A multidisciplinary approach, including the use of mass media, is required to create awareness about BSE and to reach a broader community.
Keywords: Knowledge of Breast self-Examination, Attitude towards breast self-Examination, Barriers to Breast self-Examination, Breast Self-Examination
Breast cancer is the most often diagnosed and the leading cause of cancer mortality among women worldwide, accounting for 23 per cent of all cancer cases and 14 per cent of cancer deaths, with an annual incidence of 3 per cent and a death rate of 1.8 per cent (Atuhairwe et al., 2018).
According to the World Health Organization, it is estimated that 2.3 million women were diagnosed with breast cancer globally in 2020, of which 685,000 succumbed to breast cancer (WHO, 2021). The annual estimates of age-standardised incidence rates per 100,000 women in Sub-Saharan Africa and Eastern Africa were 33.8 and 30.4, respectively (Azubuike et al., 2018). In 12 Sub-Saharan African nations, 5-year age-standardised relative survival was 66 per cent for cases detected between 2008 and 2015, compared to 85 per cent to 90 per cent for cases diagnosed in high-income countries between 2010 and 2014 (Sung et al., 2021). Eastern Africa has a breast cancer mortality rate of 15.4 per 100,000, with a 5-year breast cancer survival rate of 37.7 per cent, compared to 35.2 per cent and 48.1 per cent in West Africa and South Africa, respectively (Popli et al., 2022).
The age-standardised incidence and death rates of breast cancer in Uganda, a low-income nation, are 21.3 per 100,000 population and 10.3 per 100,000 population, respectively, which shows that almost a half of Ugandan women diagnosed with breast cancer will die from the disease (Scheel et al., 2020). Among women diagnosed with breast cancer in Uganda, 89 per cent present at stage III or IV, which is more difficult to treat and has poor prognosis (Scheel et al., 2020).
Mammography, clinical breast examination (CBE) and breast self-examination (BSE) are the most essential strategies for early identification of breast cancer. Mammography has long been considered the best option for early detection of breast cancer since it can detect the disease even before the woman notices a lump; however, because of its high cost and limited availability, this strategy is limited in developing countries (Boafo and Tetteh, 2020).
Early detection of the cancer when it has not spread to other parts of the body makes treatment more effective and increases the patient’s quality of life and chances of survival. The most reliable and cost-effective strategy to detect breast cancer early is to have frequent BSEs (Alshahrani et al., 2020). BSE is a non-invasive procedure in which women examine their breasts on a monthly basis between the seventh and tenth day of the menstrual cycle in order to discover any abnormal swelling or lumps; this enables them to seek medical help as soon as possible (Birhane et al., 2017).
There is still a gap in early identification of breast cancer in Uganda. As such, women are seen to present with the disease in late stages, which probably could be attributed to lack of knowledge on BSE. Few studies have been published about knowledge, attitudes and barriers to BSE in Uganda and none in West Nile and in Arua City. The objective of this study is to assess the knowledge, attitudes and barriers to BSE among women in Nyio ward, Arua City.
A descriptive cross-sectional study was conducted using quantitative methods.
Nyio ward is located in Arua City, Uganda. As of the Uganda Bureau of Statistics (UBOS) 2020 projections, Arua had a population of 751000 with 52% being females The Illiteracy status rate in Arua is high at over 72 per cent among individuals aged ten years and above. There are two divisions in Arua City: Ayivu and Arua Central Division with 26 sub-counties. Most people in Ayivu Division are Christians, while the majority in Arua Central Division are Muslims.
Arua City comprises different ethnicities and races, such as the Lugbara, Alur, Kakwa, Madi, Indians, Sudanese, Congolese, Bantu, Langi and Acholi. Nyio ward has six villages – namely, Awulaka/Olivu, Aroyi, Muni, Nyio, Ofude and Ogayi, and the dominant tribe is Lugbara, which is their local language. Small-scale farming is done on fertile soils especially near the valleys and the slopes of the hills.
This included all females aged aged 18 years and above living in Nyio ward, Arua City.
The subjects of this study were women who had been living in Nyio ward for the past 3 years, aged 18 years and above, had never suffered from breast cancer, and signed the consent form so as to participate out of their own free will.
Those who were excluded from this study were women who were critically ill, mentally ill or had travelled out of the ward on the day of data collection.
The sample size was estimated using the formula developed by Kish and Leslie (1965). Considering the reported prevalence of 35.2 per cent of women who knew how to perform breast self-examination in a study carried out in Kyadondo County (Atuhairwe et al., 2018):
where:
N = Minimum required sample size
Z = Standard normal variable at (1-α) % confidence level and, α is mostly 5%, with 95% confidence level (standard value of 1.96)
D = Precision/margin of sample error -/+5%
P = Proportion prevalence of women who knew how to perform BSE 35.2%
Q = (1 – P) = 1-35.2% = 0.648
N =
N = 350.501 N= Approximately 351 participants.
Therefore, 59 participants were obtained from each of the six villages, which made a sample size of 354 participants.
A cluster sampling method was used in this study, starting with simple random sampling to select the sub-county and ward for the study. Among the 26 sub-counties, Oluko sub-county was randomly selected. Oluko sub-county had nine wards – namely, Ambeko, Anipi, Bunyu, Nyio, Ombokoro, Onzivu, Turu, Wandi and Yabiavoko. These wards were written on different pieces of paper and chosen randomly to select only one ward (Nyio ward). Participants were obtained from all the six villages in Nyio ward. Out of the 654 households in Nyio ward, the households which participated in the study were obtained by spinning a bottle in the village centre. Where the bottle top faced was the direction the researcher and the research assistants chose for data collection. We chose 59 participants to be studied studied from each of the six villages, making a total of 354 participants.
After being granted permission by the administrators of Muni University, data was then collected. The principal investigator hired research assistants who were pursuing a bachelor’s degree in nursing, and knew both Lugbara, the local language, and English. The research assistants were trained for 2 hours about the research topic, data collection tools, and obtainig informed consent. Before data collection, the principal investigator and the research assistants first sought permission from the Local Council I (LCI) of the villages. Thereafter the principal investigator and the research assistants were given Guides from each village to take them to the households.
Households were counted following a straight line until the village boundary. A number was chosen randomly between one and the total number of houses counted. The number of the house selected randomly was the first house which was surveyed. Subsequent households were chosen by continuing away from the village centre. Only houses on the left side of the road were included. The research assistants would turn left each time a road was encountered on the left side. This was continued until all the 59 participants were obtained.
Every component of the research was explained to the participants, including the objectives of the study, the benefits, any negative effects and what was expected from them. Verbal and written consent was obtained from the participants to take part in the study by the research assistants. Participants who met the eligibility criteria were interviewed using interviewer-administered questionnaires with both open and closed questions after establishment of a rapport in a quiet environment. Each participant took a maximum of 20 minutes to answer the questions in the questionnaire.
Every participant was thanked by the research assistants after the questionnaire had been filled. Then the research assistants moved on to the next house until the desired sample size was attained. All research assistants returned the questionnaires to the principal investigator after data collection to work on the data management process. Data collection in each village was done over 2 days, during which 29 participants were interviewed on the first day and 30 on the second day.
The completed questionnaires were identified by numbering them from 1 to 354 and entered in Microsoft Excel.
Once collected data was entered into Microsoft Excel, it was cleaned, coded and imported to SPSS version 23 statistical package for analysis. Univariate analysis was used for data analysis using mean (standard deviation), frequencies and proportion for categorical variables.
Statistical frequency distribution tables, graphs and charts were used for data presentation in terms of proportions, absolute values and percentages.
Different measures of data quality control were applied to ensure validity and reliability of the data that was collected.
Reliability: The principal investigator and the research assistants carried out a pre-visit and a pre-test of the questionnaire before data collection and editing of work at the end of each data collection day to ensure its reliability (Polit and Beck, 2017). A pre-testing survey was conducted, and 30 participants were selected to take part (Perneger et al., 2015). Ten participants were obtained by convenience sampling from each of Awindiri, Ayibiri and Euata villages within Onzivu ward making a total of 30 participants. Questions were developed according to the objectives and reviewed literature.
Validity: A content validity index (CVI) was used to test the questionnaire’s validity, as shown in the formula below.
A minimum of 0.75 of content validity index was used to confirm validity (Lawshe, 1975). The questionnaire was translated into Lugbara, the local language spoken by the majority of Nyio ward women.
The research assistants were bachelor’s degree holders of nursing and fluent in both Lugbara and English languages.
Participant’s responses were recorded as soon as they were given. After the interviews were completed, the researcher double checked all of the questionnaires for accuracy before storing them.
Ethical clearance was obtained from the Department of Nursing and Midwifery, Muni University. Authorisation to conduct the study in Nyio ward was obtained from the Town Clerk and from the Local Council of one of each of the villages.
Study participants had to consent by signing/ putting a thumbprint on the on written consent forms and questionnaires were anonymised.
A total of 354 females – 16.7 per cent from each village – responded to the questionnaire with a response rate of 100 per cent. The mean age of the respondents was 29 years. The minimum age was 18 years while the maximum was 83 years. The majority of the respondents were of the Lugbara tribe (90.1 per cent); 47.2 per cent were Catholics and more than half (54.2 per cent) were married. In terms of education, the largest proportion stopped at primary education (39.8 per cent), 37.0 per cent had informal occupations and 31.1 per cent had no children, as shown in Table 1.
| Variable | Frequency | Percentage % | Age group in years |
| 18-28 | 213 | 60.2% |
| 29-39 | 83 | 23.4% |
| 40-50 | 42 | 11.9% |
| 51+ | 16 | 4.5% | Tribe |
| Lugbara | 319 | 90.1% |
| Madi | 8 | 2.3% |
| Kakwa | 13 | 3.7% |
| Alur | 6 | 1.7% |
| Others | 8 | 2.3% | Religion |
| Catholic | 167 | 47.2% |
| Islam | 22 | 6.2% |
| Protestant | 156 | 44.1% |
| Other | 9 | 2.5% | Marital status |
| Single | 120 | 33.9% |
| Married | 192 | 54.2% |
| Divorced | 23 | 6.5% |
| Widowed | 19 | 5.4% | Level of education |
| None | 53 | 15.0% |
| Primary | 141 | 39.8% |
| Secondary | 77 | 21.8% |
| Tertiary | 83 | 23.4% | Occupation |
| House wife | 83 | 23.4% |
| Formal | 62 | 17.5% |
| Informal | 131 | 37.0% |
| Student | 78 | 22.0% | Number of children |
| 0 | 110 | 31.1% |
| 1-2 | 107 | 30.2% |
| 3-4 | 77 | 21.8% |
| 5-6 | 50 | 14.1% |
| 7+ | 10 | 2.8% |
Most of the respondents (96.6 per cent) had heard about breast cancer although only 16.7 per cent had ever had a family member diagnosed with breast cancer. Less than half of the respondents (47.5 per cent) reported having heard about Breast Self-Examination (BSE) as a means of early detection of breast cancer. Only 23.2 per cent (n=39) of the 168 respondents who had heard of BSE knew how to perform the examination. Out of the 39 respondents who knew how to perform BSE, 13 (33.3 per cent) knew when to perform BSE and only 3 (7.7 per cent) correctly reported the five major steps of BSE. A few of the 354 women (20.1 per cent) reported knowing how to identify lumps in the breast. (See Table 2.)
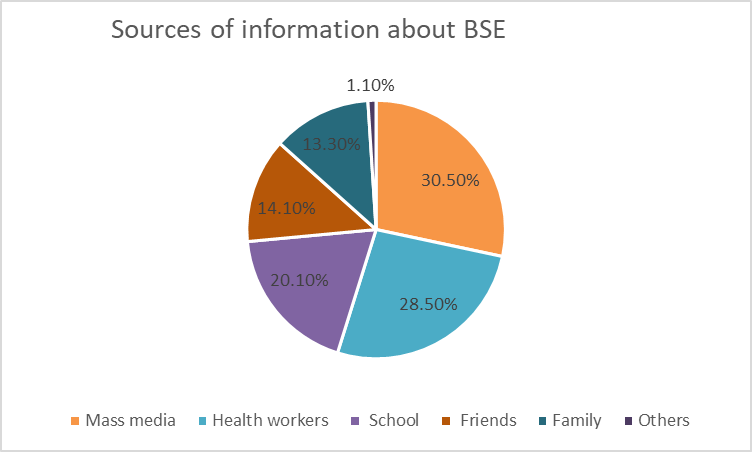
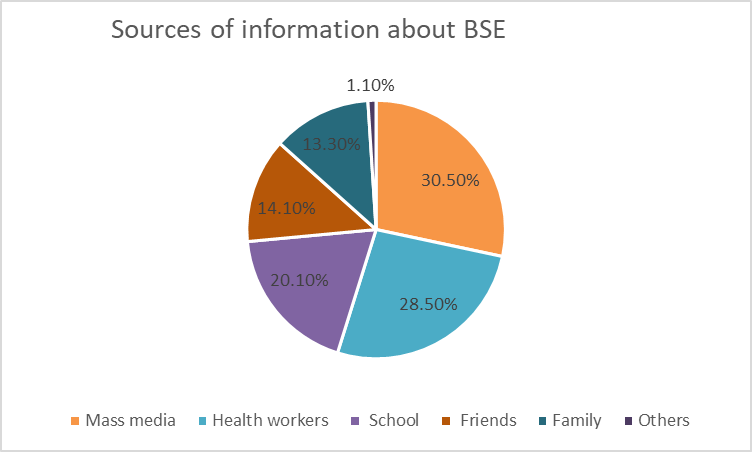
Among the 13 respondents who reported knowing when to perform BSE only 9 (69.2 per cent) reported correctly that it is performed ‘after menstruation’. One person (7.7 per cent) reported ‘anytime’, 1 (7.7 per cent) reported ‘every three months during pregnancy’ and 2 people (15.4 per cent) reported ‘before menstruation’ (See Table 3). Figure 1 shows that out of the 168 respondents who had heard about BSE, 30.5 per cent obtained the information from mass media (News, Radio or Television, WhatsApp, Twitter) and some had more than one source of information. Other sources of information were through community talks and gatherings.
| Variable | Frequency | Percentage % | |
| Heard of breast cancer |
YES NO |
342 12 |
96.6% 3.4% |
| Ever had a family member diagnosed with breast cancer |
YES NO |
59 295 |
16.7% 83.3% |
| Heard of BSE as means of early detection of breast cancer |
YES NO |
168 186 |
47.5% 52.5% |
| Know how to perform BSE |
YES NO |
39 129 |
23.2% 76.8% |
| Know when to perform BSE |
YES NO |
13 26 |
33.3% 66.7% |
| Know the 5 major steps of BSE |
YES NO |
3 36 |
7.7% 92.3% |
| Know how to identify lumps |
YES NO |
71 283 |
20.1% 79.9% |
| If yes, when to perform BSE | Frequency | Percentage % |
| After menstruation | 9 | 69.2% |
| Anytime | 1 | 7.7% |
| Every three months during pregnancy | 1 | 7.7% |
| Before menstruation | 2 | 15.4% |
In Figure 2, out of the 168 respondents who had heard of BSE as a means of early breast detection, the majority of the respondents (95.8 per cent) had a positive attitude that BSE is a good practice and believed all women should examine themselves. Many respondents (41.7 per cent) agreed they would perform BSE if they had any risk of breast cancer, 29.2 per cent said they would if there was a cure and 28.0 per cent agreed they would perform BSE if their family approved it. The largest proportion (85.7 per cent) were positive that BSE is important and useful to detect breast cancer early and most (83.3 per cent) believed early detection increases the chance of long-term survival. Less than a half (25.0 per cent) of respondents believed that BSE is not necessary to perform if one has no problems with the breasts. A few (19.6 per cent) of the respondents felt that BSE should only be performed by women over 20 years. A few (3.6 per cent) acknowledged that they did not like to practice BSE because they were afraid – they may discover breast cancer in themselves – while 7.1 per cent did not like to practice BSE even though they were fully aware of its benefits. Only 18.5 per cent reported that performing BSE made them feel funny, or unpleasant, disgraceful and embarrassed because it requires them to touch their breast. All respondents reported they would go to the health facility if there were any symptoms of breast cancer.
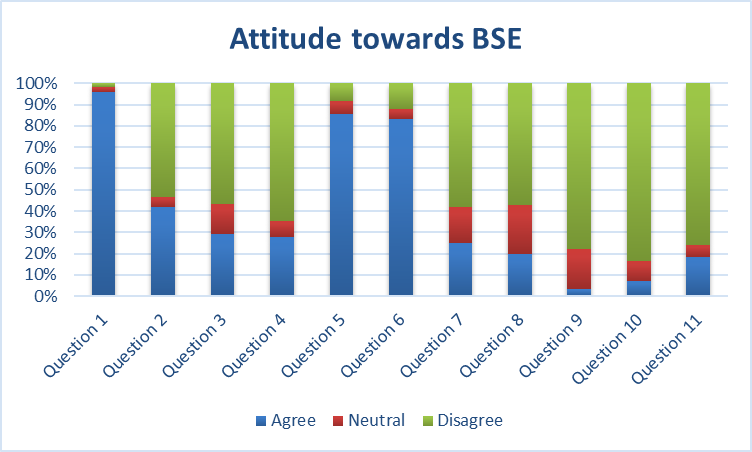
Question 1: BSE is a good practice
Question 2: Perform BSE if having a risk
Question 3: Perform BSE if there was a cure
Question 4: Perform BSE if family approve
Question 5: BSE is good to detect breast cancer early
Question 6: Early detection, high chance of survival
Question 7: BSE not needed if no problems with breast
Question 8: BSE for women over 20 years
Question 9: Afraid to discover breast cancer
Question 10: Know it's benefits but don't like to practice BSE
Question 11: Funny, unpleasant, disgraceful and embarrassing to touch breast
Table 4 shows that, out of the 354 participants, the majority (92.4 per cent) lacked awareness about BSE technique. Less than a half (28.2 per cent) lacked self-confidence, and a few (12.4 per cent) had discomfort with breast manipulation. Half (50.3 per cent) of the respondents never knew the importance of BSE while 47.7 per cent reported low education levels on the subject. A high proportion (74.0 per cent) of respondents reported lack of advice from health care workers to perform BSE, 31.6 per cent were afraid of touching lumps and detecting breast cancer and a few (15.5 per cent) had forgetfulness. Only 28.2 per cent reported negligence and 44.4 per cent lacked time to practice BSE. Most respondents (79.4 per cent) did not receive trainings from health facilities and 17.2 per cent were afraid of pain during BSE.
|
Barriers towards BSE |
Frequency | Percentage % | |
| Lack of awareness about BSE technique |
YES NO |
327 27 |
92.4% 7.6% |
| Lack of self-confidence |
YES NO |
100 254 |
28.2% 71.8% |
| Discomfort with breast manipulation |
YES NO |
44 310 |
12.4% 87.6% |
| Not knowing the importance of BSE |
YES NO |
178 176 |
50.3% 49.7% |
| Low education level |
YES NO |
169 185 |
47.7% 52.3% |
| Lack of advice from health care workers |
YES NO |
262 92 |
74.0% 26.0% |
| Fear of touching lumps and detecting breast cancer |
YES NO |
112 242 |
31.6% 68.4% |
| Forgetfulness |
YES NO |
55 299 |
15.5% 84.5% |
| Negligence |
YES NO |
100 254 |
28.2% 71.8% |
| Lack of time |
YES NO |
157 197 |
44.4% 55.6% |
| Lack of training from health facilities |
YES NO |
281 73 |
79.4% 20.6% |
| Fear of pain during BSE. |
YES NO |
61 293 |
17.2% 82.8% |
| Others |
YES NO |
3 351 |
0.8% 99.2% |
The study findings indicate that few participants were aware of breast self-examination as a means of early detection of breast cancer. This outcome is supported by the findings of Suleiman (2014), a study conducted among Jordanian women which showed that only 34.9 per cent were aware of BSE as a means for early detection. This may have been because of the low levels of education attained by the women who participated in the study. In addition, Joyce et al. (2020) found that knowledge of BSE was low (39.4 per cent) among 386 women above 18 years in Eastern Uganda. Since this paper shows that most participants stopped at primary level of education, it was possible that they would have low awareness about BSE compared to other populations. The study conducted among nursing and clinical nutrition students in Gaza indicated conflicting findings that the vast majority of respondents (96.5 per cent) had a high knowledge about BSE Abo Al-Shiekh et al., 2021. This could have been because these students were taught in medical schools, thus they may have had prior sessions about BSE. The results obtained emphasise the need for increased awareness and promotion of BSE practices among women, particularly in regions with limited access to healthcare services.
As seen in Figure 1, the main source of information given to participants was through mass media, followed by health workers. This is in agreement with a retrospective study carried out in Saudi Arabia among 508 participants which revealed that more than half of the participants (53.62 per cent) obtained the information about BSE through social media and 18.84 per cent through the medical staff (Alshahrani et al., 2020). Our study findings were contrary to the findings of the study carried out in Eastern Uganda Joyce et al., (2020), which revealed that health workers were the primary source of information (55.9 per cent) followed by News/media (23 per cent). The differences in findings may be due to the study setting since the study was conducted in a hospital, which may have introduced biases among respondents. Although health workers remain a crucial source of information, making use of mass media can increase awareness and reach a broader audience – especially in rural communities.
Only a few respondents (11 per cent) knew how to perform BSE; this is contrary to the study done by Joyce et al. (2020), which showed that 58.6 per cent of the respondents knew how to perform BSE. Among those who knew how to perform BSE, less than half of the respondents stated correctly that BSE should be performed a week after the start of menses. This is different from the findings of Abo Al-Shiekh et al. (2021) who studied knowledge of female nursing and clinical nutrition university students, which revealed that 69.8 per cent knew when to perform BSE. This is probably because nursing and clinical nutrition students may have heard about BSE from school and the training hospitals, and they are more sensitised in terms of disease and its preventive measures. Also, according to Joyce et al. (2020), only a few of the respondents (11.8 per cent) reported correctly that it should be done one week after menstruation.
The findings of this study indicated that only three of the respondents reported correctly the five major steps of BSE. The study findings of Abo Al-Shiekh et al. (2021) revealed that 22.1 per cent of the respondents could correctly apply the steps of BSE. In another survey conducted among 308 students from the University of Ghana, 98.7 per cent students admitted that they were sure of the steps to follow during BSE and could identify a lump by performing BSE (Boafo and Tetteh, 2020). From the reviewed literature, most of the studies did not attempt to assess the exact steps of BSE among the participants. Therefore, it cannot be concluded whether the participants knew the five major steps of BSE. Twenty percent of respondents in this study reported knowing how to identify lumps in the breast. This is less than the findings of Atuhairwe et al. (2018) in a household survey of women in Kyadondo County, Central region, Uganda, which showed that 35.2 per cent of the women knew how to check their own breasts for lumps. The findings suggest that there is need to pay attention to steps involved in BSE and how to identify lumps during training sessions.
Findings in this study showed that most participants agreed BSE is a good practice for all women. This is similar with the findings of a study conducted among 420 female university students in Ethiopia which revealed that most of the study participants (96.5 per cent) agreed that BSE is important and beneficial for detecting breast cancer (Birhane et al., 2017). Another in study in Saudi Arabia that surveyed 508 participants revealed similar results where 95.28 per cent of the respondents agreed that early identification of breast cancer boosts the likelihood of recovery (Alshahrani et al., 2020). Through BSE awareness, most misconceptions about breast cancer and BSE can be cleared, ultimately promoting its practice and contributing to better health outcomes.
Although the majority of the participants agreed that BSE was a good practice, few did not like to practice it despite being fully aware of its benefits. A greater proportion believed that BSE is important and useful to detect breast cancer early, and that early detection increases the chance of long-term survival. This is similar to the study by Birhane et al. (2017) which showed that 89.9 per cent of the respondents believed that early identification increases the chances of long-term survival. Also, the findings by Alshahrani et al. (2020) revealed that 95.28 per cent of the respondents believed early identification of breast cancer boosts the likelihood of recovery. By encouraging women to practice BSE, healthcare providers can empower them to take proactive steps towards early detection and treatment, potentially improving breast cancer outcomes.
In our study, not many women would practice BSE if their family did not approve it and only a few would practice it only if there was a known cure for the disease. This is similar with the findings of Suleiman (2014) who found that 25.5 per cent of the respondents would practice BSE if their family approved and 19.3 per cent only if there was a known cure for \the disease in a study he conducted among 900 female Jordanian students from the University of Jordan in Amman. The participants in his study were enrolled voluntarily, which could have made the results biased and the students who chose to participate may have had different attitudes towards BSE than those who did not volunteer.
Hardly any participants acknowledged fear of discovering breast cancer in themselves. Similar findings were obtained by Waswa (2017) in a study among women aged 18–45 years in gynaecological ward at KIU-teaching hospital in Uganda which revealed that most (75 per cent) of the participants feared being diagnosed with breast cancer and thus did not perform BSE. In this study, few (25.0 per cent) reported it was not necessary to perform BSE for those who had no breasts problems, which is similar to the findings of the same study by Waswa (2017 with 11.5 per cent of participants believing that it was not necessary if one had no problems with the breast. A small number reported feeling funny, unpleasant, disgraceful and embarrassed while preforming BSE. This is contrary to the findings of Waswa, 2017 where none of the participants reported the above with BSE practice. The differences in the results may be because the current study was conducted in villages whereas Waswa’s study was conducted in a hospital and a more urban setting, therefore a practice of wellness could not have been considered funny, unpleasant, disgraceful and embarrassing. The findings also suggest that women in rural settings may face unique barriers when practicing BSE, which may need to be addressed through targeted education and awareness efforts.
In our study, few (19.6 per cent) respondents believed BSE should only be performed by women over 20 years. Meanwhile Alshahrani et al., 2020 reported that 76.18 per cent of the participants agreed that women over the age of 20 should conduct BSE. This could have been due to limited knowledge about BSE among the participants in the current study, thus they may have not known the right age for performing BSE regularly.
All of the respondents said they would visit a health facility if they noticed any signs of breast cancer. Similar results were obtained by Birhane et al. (2017) who found that nearly all respondents (96.8 per cent) stated they would visit a health facility if they experienced any signs or symptoms of breast cancer.
In this study, the majority of the participants reported a lack of awareness about BSE technique, a few lacked self-confidences, a minority had discomfort with breast manipulation and more than half the respondents didn’t know about the importance of BSE. In line with these findings, a study carried out among 52 women in Kampala, Uganda revealed that more than a half (65 per cent) did not practice BSE due to lack of information about how to perform BSE, 15 per cent lacked self-confidence and a few (10 per cent) had discomfort with breast manipulation (Waswa, 2017). On the other hand, only 8 per cent of the participants in the same study didn’t know the importance of examining breasts (Waswa, 2017). These findings highlight the necessity of including breast cancer screening techniques in the sensitisation sessions by healthcare providers and regularly raising community awareness of BSE and its advantages.
Almost half of the participants in our study with low education level had no access to information about BSE, thus hindering their practice. This is consistent with the findings of Shakti Yambem and Rahman (2019) who surveyed 302 Sikkimese women in India. Their study revealed that education level is among the significant predictors of BSE. Out of the 302 women, 172 women had a low education level (<12th standard) and 130 women had a high education level (>12th standard). Those with a low education level showed 9.3 per cent of women who had practiced BSE and 90.7 per cent who had never self-examined. Of those with a high education level, 31.5 per cent had practised BSE and 68.5 per cent had never self-examined (Shakti Yambem and Rahman, 2019). Women who had attained a higher education level embraced BSE practice due to a prior awareness compared to those who did not.
The results from our study showed that a few of the respondents cited forgetfulness, negligence as reasons why they did not practise BSE. Almost half lacked time to self-examine, most reported a lack of advice from health care workers to perform BSE and the majority did not receive trainings from health facilities. Not many of the participants were afraid of touching lumps and detecting breast cancer and only a few were afraid of experiencing pain during BSE. Consistent with these results, a study by Taleghani et al. (2019) of 202 Iranian women from rural areas in Isfahan city, 21.30 per cent women mentioned lack of awareness about BSE techniques, 37.60 per cent cited forgetfulness and negligence, 25.7 per cent reported a lack of time or being too busy, 8.90 per cent were afraid of touching lumps and detecting breast cancer and only 8.40 per cent were afraid of pain during BSE. The same study reported that only 13.40 per cent mentioned lack of training by health care workers, which does not correlate with the findings of our study. In another study some women blamed their family physician for not advising them to perform BSE (Shakti Yambem and Rahman, 2019).
Despite the study by Taleghani et al. (2019) being conducted in the suburbs of the city, only 5.3 per cent of the women were illiterate compared to the current study where 15.0 per cent had never gone to school. Education level is significantly associated with some barriers to BSE. Women having a high education level were more likely to practise BSE than those with lower education, and women with lower levels of education also have poor understanding of behaviours associated with early detection of breast cancer. The specific demographic characteristics of women should be taken into account while designing nursing strategies and interventions to prevent BSE.
There is also a need to make individualised approaches to handle factors that may hinder BSE practice among women.
The research findings were disseminated to the faculty of health sciences in the department of Nursing and Midwifery of Muni University. Results from the study were submitted to Muni University as a partial fulfilment of the requirement for the award of a bachelor’s degree in nursing and Nyio community through a meeting. It was also presented in the WorldCUR-BCUR conference 2023 at the University of Warwick in United Kingdom.
Most variables were measured by the participants’ subjective report which may have led to introduction of observation and recall bias. BSE was explained to some participants who raised questions, thus some of the findings could have been affected due to having prior information.
Despite a significant proportion of participants having heard about breast cancer, and having a positive attitude towards Breast Self-Examination, BSE practice is still very low. Lack of awareness is a primary barrier towards BSE practice highlighting a need for health professionals to raise community awareness about BSE, its significance, techniques and steps involved.
Health workers are urged to implement BSE health education programmes within the healthcare facilities. Since most women in rural areas have access to mass media such as radios, it is recommended to promote public breast health awareness campaigns through the media.
There is a need to conduct research to assess the impact of women’s demographics like age, level of education and economic status on BSE practice.
I give thanks to Allah, the Almighty, for giving me life grace and strength throughout my studies.
I thank all the friends that I have met here at Muni University for their continued assistance and support whenever possible, throughout this study.
To all my lecturers in the faculty of health science, you all added a lot of value and knowledge to my life inside and outside campus.
I appreciate all the participants who agreed to take part in the study and their compliance throughout the data collection process.
My special thanks go to my father Ibuuza Hamzah, my mother Namugawe Fatuma and my siblings who gave me a hand in times of need.
Ms. Aleni Mary, my supervisor, deserves my heartfelt gratitude and gratefulness for her direction, patience and competent supervision during the research work; may the Lord bless you and your family abundantly.
Table 1: Socio-demographic characteristics of study participants in Nyio ward
Table 2: Knowledge of breast self-examination among females in Nyio ward
Table 3: Responses from participants who stated knowing when to perform BSE
Table 4: Barriers towards BSE practice among women in Nyio ward
Figure 1: Showing the sources of information about BSE among females in Nyio ward
Figure 2: Showing the Attitude of females in Nyio ward towards Breast-self examination
Investigator’s Name: _______________________
Student number: ___________________________
Address: Muni village, Nyio ward, Oluko Subcounty, Arua City
I am asking for your voluntary participation in my research project. Please read the following information about the study.
Research Title: Knowledge, Attitude and Barriers of Breast Self-Examination Among Women in Nyio Ward, Arua City
Study objective
To assess knowledge, attitude and barriers of breast self-examination among women in Nyio ward, Arua City.
Purpose of the study
This research will generate information which will be used by health facilities and community health services to create awareness about breast cancer and the basic screening services available. This study will encourage the women within the community to understand and practice BSE such that in case of any unusual breast findings they report early to the health care facilities for prompt management, thus reducing breast cancer morbidity and mortality.
Health workers might also be encouraged to pay more attention to clinical breast examination and teach women how to perform BSE especially where there are identified risk factors. This study will also guide future researchers on the different aspects to study about which may affect BSE practice among the different communities.
If you accept to participate, you will be asked to:
Give honest and truthful responses to all the questions in the questionnaire. You will not be judged for the answers you submit but the investigator and research assistant will offer guidance where necessary to clear any misconceptions
Benefits of participating in the study
There will be no direct benefits for participation; however, the findings will be presented to Nyio community through a meeting. It will also be presented in conferences, seminars and workshops, published in scientific journals and social media platforms like Facebook, WhatsApp and Twitter.
Risks
We do not anticipate any risks in this study, but some questions might have negative mental effects during in some individuals.
How confidentiality will be maintained
This study has been approved by the Department of Nursing and Midwifery in partial fulfilment of the award of bachelor degree in nursing sciences at Muni University. It will be conducted according to the ethical guidelines and principals. Only the researcher will have access to the data obtained in this study and the questionnaires will be kept in a locked place to prevent unauthorised persons from accessing them. The participant’s identity will remain anonymous in any report on the results of this research. This will be done by giving questionnaires numbers from 1 to 354.
If you would like to participate, please sign in the box below.
Voluntary Participation:
Participation in this study is completely voluntary. If you decide not to participate there will not be any negative consequences. Please be aware that if you decide to participate, you may stop participating at any time during the course of the study and you may decide not to answer any specific questions.
I understand that I am free to contact any of the people involved in the research to seek further clarification and information about names, degrees, affiliations and contact details of researchers (and academic supervisors when relevant).
By signing this form, I am attesting that I have read and understand the information above in the language I understand and I freely give my consent to participate in this study.
Participant’s Name _____________________________ Signature/thumb print______________________
Date Consented _____________________________
If you have any questions about this study, feel free to contact;
Telephone: _______________________ Email: _______________________
Signature of researcher
I believe the participant is giving informed consent to participate in this study.
Signature of researcher and Date: ________________________________________
A Questionnaire to Study the Knowledge, Attitude and Barriers of Breast Self-examination among women in Nyio ward
PART ONE: Socio-demographics
Circle one of the options for the questions below and fill in where appropriate
Age: _______________________ Tribe: _______________________
Religion: a) Catholic b) Islam c) Protestant d) Others, please specify_______________________
Marital status: a) single b) married c) divorced d) widowed
Level of education: a) None b) Primary c) Secondary d) Tertiary
Occupation:_______________________
Place of residence (village): _______________________
Number of children: __________
PART TWO: Knowledge about Breast Self-examination (BSE)
Circle one of the options for the questions below and write where appropriate
Have you ever heard of breast cancer?
a) YES b) NO
Do you have any family member who was diagnosed with breast cancer?
a) YES b) NO
Have you ever heard of Breast Self-examination as a means of early breast cancer detection?
a) YES b) NO
Do you know how to perform Breast Self-examination?
a) YES b) NO
Do you know when Breast Self-examination is supposed to be performed?
b) YES b) NO
If YES, when should Breast Self-examination be performed?
_____________________________________________________________________
Do you know the five major steps of breast self-examination?
a) NO b) YES
Do you know how to identify lumps in the breast during breast self-examination?
a) NO b) YES
What sources of information do you have for Breast Self-examination? Circle all that apply
a) Mass media (News, Radio or Television, WhatsApp, Twitter)
b) Health workers
c) School
d) Friends
e) Family
f) Others, Please specify
PART THREE: Attitude towards Breast Self-examination (BSE)
For this part, indicate a tick below the different responses (chose one in each section)
| Questions | Response | ||||
| Strongly disagree (1) | Disagree (2) | I do not Know (3) | Agree (4) | Strongly agree (5) | |
| Breast self-examination is a good practice; therefore, all women should practice it | |||||
| I would perform BSE if I had any risk factor to breast cancer | |||||
| I would perform BSE if there was a known cure to breast cancer | |||||
| I would perform BSE if my family approved it | |||||
| BSE is important and useful to detect breast cancer early | |||||
| Early detection will increase the chance of long-term survival | |||||
| BSE is not necessary to perform if one has no problems with the breasts | |||||
| BSE is supposed to be performed by women over 20 years | |||||
| I do not like to practice BSE because I am afraid that I may discover breast cancer on myself | |||||
| I do not like to practice BSE even though am fully aware of its benefits | |||||
| Performing BSE makes me feel so funny, or unpleasant, disgraceful and embarrassed because it makes me touch my breast | |||||
Where would you go, if there are any symptoms of breast cancer?
a) Health facility
b) Traditional healer
c) Hide it
d) Other, Please specify
____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
PART FOUR: Barriers towards Breast Self-examination (BSE)
What are the reasons that prevent you from performing Breast Self-examination? Circle all that apply
a) Lack of awareness about BSE technique
b) Lack of self-confidence
c) Discomfort with breast manipulation
d) Not knowing the importance of BSE
e) Low education level
f) Poor socio-economic status
g) Lack of advice from health care workers
h) Fear of touching lumps and detecting breast cancer
i) Forgetfulness
j) Negligence
k) Lack of time
l) Lack of training from health facilities
m) Fear of pain during BSE
n) Others, please specify below
___________________________________________________________________________________________________________________________________________________________________________________________________________________________
Al-Shiekh. A, S. Samira., M. A, Ibrahim., and Y.S. Alajerami, (2021), ‘breast cancer knowledge and practice of breast self-examination among female university students, Gaza’, Scientific World Journal, 2021(1), p.6640324 https://doi.org/10.1155/2021/6640324
Alshahrani, S. M., A. Almutiran, and N. J Ahmed,. (2020), ‘Awareness and attitudes regarding breast self-examination and breast cancer among females in Alkharj’, Journal of Pharmaceutical Research International, 32 (26), 71–77. https://doi.org/10.9734/jpri/2020/v32i2630840
Atuhairwe, C., D. Amongin, E. Agaba,S. Mugarura, and I. M. Taremwa, (2018), ‘The effect of knowledge on uptake of breast cancer prevention modalities among women in Kyadondo County, Uganda’ 18 (1), 279. https://doi.org/10.1186/s12889-018-5183-5.
Azubuike, S. O., C. Muirhead, L. Hayes, and R. McNally, (2018), ‘Rising global burden of breast cancer: The case of Sub-Saharan Africa (with emphasis on Nigeria) and implications for regional development: A review’, World Journal of Surgical Oncology, 16 (1), 1–13. https://doi.org/10.1186/s12957-018-1345-2
Birhane, K., M. Alemayehu, B. Anawte, G. Gebremariyam, R. Daniel, S. Addis, T. Worke, A.Mohammed, and W. Negash, (2017), ‘Practices of breast self-examination and associated factors among female Debre Berhan university students. 2017. International journal of breast cancer, 2017(1), 8026297
Boafo, I. M., and P. M. Tetteh, (2020), ‘Self-efficacy and perceived barriers as determinants of breast self-examination among female nonmedical students of the University of Ghana’, International Quarterly of Community Health Education, 40 (4), 289–297. https://doi.org/10.1177/0272684X19885501
Joyce, C., L. V. N. Ssenyonga, and J.S. Iramiot, (2020), ‘Breast self-examination among female clients in a tertiary hospital in Eastern Uganda’, International Journal of Africa Nursing Sciences, 12 (November 2019), 100–186. https://doi.org/10.1016/j.ijans.2019.100186
Lawshe, C. H. (1975), ‘A quantitative approach to content validity’, Personnel Psychology, 28 (4), 563–575. https://doi.org/10.1111/j.1744-6570.1975.tb01393.x
UBOS (Uganda Bureau of Statistics) (14 June 2020). ‘The population of all Ugandan cities and towns with more than 15,000 inhabitants according to census results and latest official projections’, available at: https://www.citypopulation.de/en/uganda/cities/, accessed 18 May 2022
Perneger, T. V., D. S. Courvoisier, P. M. Hudelson, and A. Gayet-Ageron, (2015), ‘Sample size for pre-tests of questionnaires’, Quality of Life Research, 24 (1), 147–51. https://doi.org/10.1007/s11136-014-0752-2
Polit, D. F. and C. T. Beck (2017), Nursing Research (10th edt), available at https://archive.org/details/PolitD.F.BeckC.T.2017.NursingResearchGeneratingAndAssessing, accessed 13th April 2022
Popli, P., E. M Gutterman,. C. Omene, S.Ganesan, and D. Mills, (2022). ‘Receptor-defined breast cancer in five East African countries and its implications for treatment : systematic review and meta-analysis’, 289–301. JCO Global Oncology, 7 (1), https://doi.org/10.1200/GO.20.00398
Scheel, J. R., M. J. Giglou,, S. Segel, J. Orem, V. Tsu, M. Galukande, J. OkelloG. Nakigudde, N. Mugisha, Z. MuyindaB. O. Anderson, and Duggan, C. (2020), ‘Breast cancer early detection and diagnostic capacity in Uganda’, Cancer, 126, 2469–80. https://doi.org/10.1002/cncr.32890
Yusoff, M. S. B. (2019). ABC of content validation and content validity index calculation. Education in medicine journal, 11(2), 49-54.
Shakti Yambem, L. and H. Rahman, (2019), ‘Knowledge, attitudes, and beliefs about breast cancer and barriers to breast self-examination among Sikkimese women’, Indian Journal of Medical and Paediatric Oncology, 40 (2), 175–81. https://doi.org/10.4103/ijmpo.ijmpo_162_17
Suleiman, A. (2014), ‘Awareness and attitudes regarding breast cancer and breast self-examination among female Jordanian students’, Journal of Basic and Clinical Pharmacy, 5 (3), 74. https://doi.org/10.4103/0976-0105.139730]
Sung, H., J.,Ferlay, R. L. Siegel, M. Laversanne, I. Soerjomataram, A. Jemal, and F. Bray (2021), ‘Global cancer statistics 2020 : GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries’, CA A Cancer Journal for Clinicians, 71 (3), 209–249. https://doi.org/10.3322/caac.21660
Taleghani, F., M. Kianpour, & M. Tabatabaiyan, (2019). Barriers to breast self-examination among Iranian women. Iranian journal of nursing and midwifery research, 24(2), 108-112.
Waswa, M. (2017), ‘Knowledge, attitude and practices of self-breast examination among women aged 18–45 years in gynecogical ward at KIU-teaching hospital’, Research Report, Kampala International University
WHO. (2021), ‘Breast cancer’, The World Health Organization, available at https://www.who.int/news-room/fact-sheets/detail/breast-cancer, accessed 13 April 2022
5-year age standardised relative survival: This refers to the probability of being alive in 5 years after a cancer diagnosis compared with the experience of the general population
Age standardised rates: are hypothetical rates that would have been observed if the populations being studied had the same age distribution as the standard population, while all other factors remained unchanged.
Attitude: A settled way of feeling or thinking about something, typically reflected in a person’s behaviour.
Barrier: This is something/situation that makes it difficult or impossible for something to happen or be achieved.
Breast self-examination: Is a screening method used in an attempt to detect early breast cancer involving a woman her self-looking at and feeling each breast for possible lumps, distortion or swelling.
Clinical breast examination: This is the physical examination of the breastmdone by a health care provider.
Content validity index (CVI):Is the extent of a measurement tool represents the measured construct and it is considered as essential evidence to support the validity of a measurement tool such as a questionnaire for research.
Knowledge: Facts, information and skills acquired by a person through experience or education.
Local Council 1 (LC 1): This is the lowest level of local government administration responsible for governing the village
Mammography: Is a technique of using low-energy X-rays to examine the human breast for screening and diagnosis of breast cancer
Women: These are adult female human beings 18 years and above.
To cite this paper please use the following details: Nabirye, H. (2024), 'Knowledge, Attitudes and Barriers of Breast Self-Examination Among Women in Nyio Ward, Arua City', Reinvention: an International Journal of Undergraduate Research, Volume 17, Issue S1, https://reinventionjournal.org/article/view/1346. Date accessed [insert date]. If you cite this article or use it in any teaching or other related activities please let us know by e-mailing us at Reinventionjournal@warwick.ac.uk.